Baseline serum neurofilament light (sNfL) levels were increased in patients with Guillain-Barré syndrome (GBS) and were an independent predictor of 1-year functional outcome, data from Spanish patients in the ongoing prospective International GBS Outcome Study showed.
“Our study shows that sNfL levels correlate with diverse clinical, epidemiological, and electrophysiological features and associate with clinical outcomes independently of other known prognostic variables,” wrote Luis Querol, MD, PhD, of the Hospital of la Santa Creu i Sant Pau in Barcelona, and coauthors in the Journal of Neurology, Neurosurgery, and Psychiatry.
“We found a correlation between baseline sNfL levels and disease severity, in agreement with previously reported findings in other peripheral neuropathies,” they added.
“Moreover, sNfL levels can be used to set different cut-off points that discriminate patients at risk of developing mild (inability to run) or moderate (ability to walk independently) disability as well as those recovering completely (ability to run) at 1 year,” they noted. “As expected, due to the monophasic nature of GBS and the ability of sNfL to only detect ongoing axonal damage, all patients with high sNfL levels at baseline returned to normal levels at 1 year.”
Neurofilament light is a marker of axonal injury studied in multiple neurologic disorders. In 98 GBS patients who had baseline sNfL levels, researchers found:
- Baseline median sNfL level was 5 times higher in those with GBS than in 53 healthy controls (55.49 pg/ml versus 9.83 pg/ml; P<0.001).
- CSF levels of NfL were also elevated compared with controls (1,308.5 pg/ml versus 440.2 pg/ml, P=0.034) in 27 participants with CSF samples available.
- At all time points during 1-year follow-up, sNfL levels correlated with measures of disability on the GBS Disability Score (GDS) and Inflammatory Rasch-built Overall Disability Scale (I-RODS).
- At 1 year, with data from 33 patients, high baseline sNfL was associated with inability to run (OR 1.65, 95% CI 1.14-2.40, P=0.009) and a worse I-RODS score.
“NfL is probably the first of many biomarkers for peripheral nerve injury that can be measured by the current ultrasensitive technologies,” wrote Bart C. Jacobs, MD, PhD, of Erasmus Medical Center in Rotterdam, the Netherlands, in an accompanying editorial. “This study is an important step towards a new era where biomarkers are used to improve the management of GBS and other inflammatory neuropathies.”
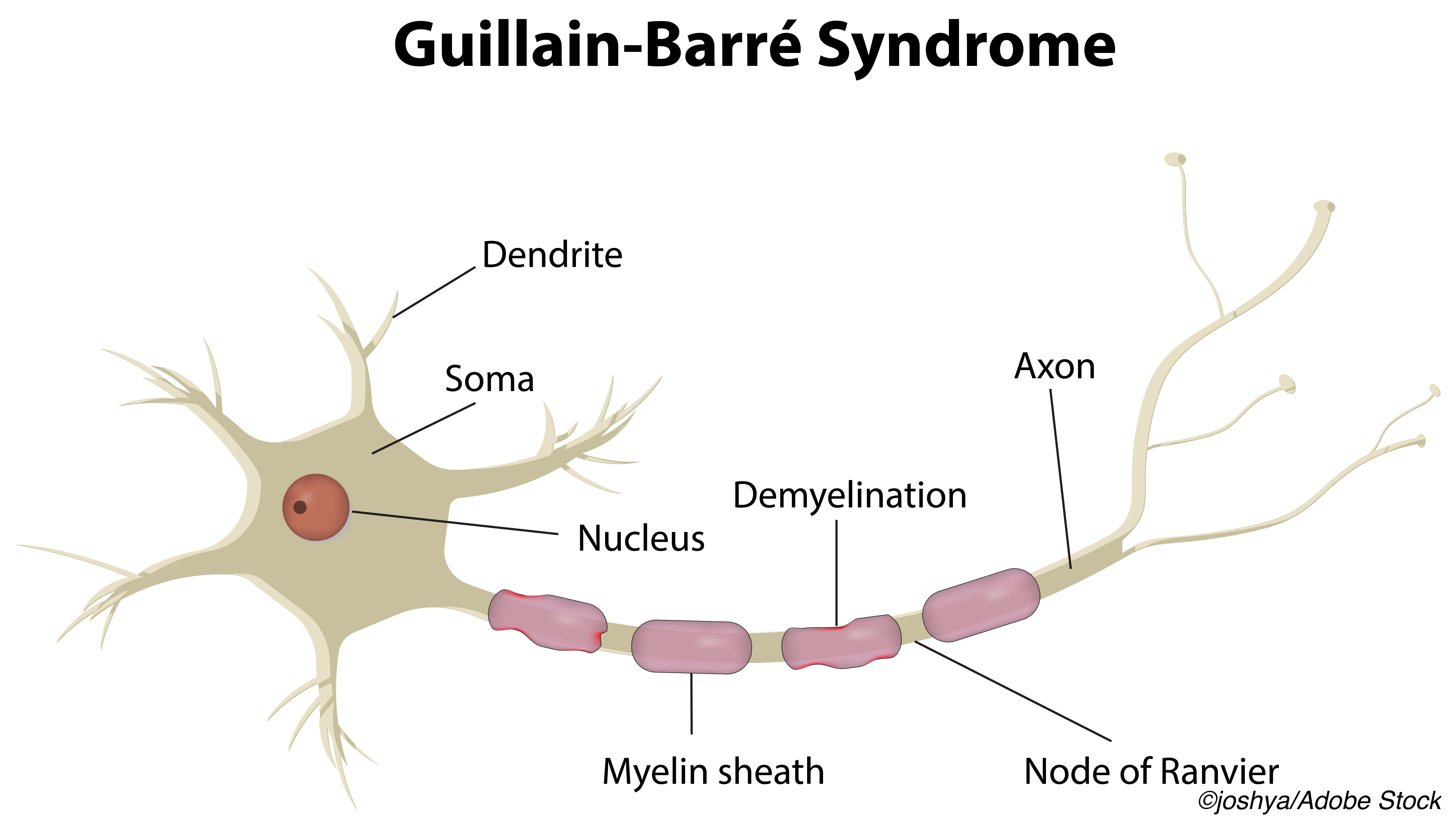
GBS is an acquired immune polyneuropathy syndrome with both demyelination and axonal degeneration. Treatment with immunoglobulins or plasma-exchange may shorten symptom duration, and prognostic models based on clinical features may be improved by biomarkers for early axonal injury.
NfL is exclusively present in neuronal cytoplasm and has been widely explored in neurologic disorders. Assays allowing extremely low levels of detection have made blood and CSF NfL attractive as diagnostic and prognostic biomarkers.
Querol and colleagues studied 98 patients in Spain from the ongoing prospective International GBS Outcome Study. Patients with GBS variants were included; the cohort had no exclusion criteria.
Clinical GBS variants were defined as sensorimotor, pure motor, pure sensory, Miller Fisher syndrome, ataxic, and pharyngeal-cervical- brachial. Nerve conduction study results were classified as acute inflammatory demyelinating polyneuropathy (AIDP), acute motor axonal neuropathy (AMAN), acute motor-sensory axonal neuropathy (AMSAN), equivocal, or normal. Disability scores were obtained at 4, 26, and 52 weeks. Known prognostic clinical factors incorporated into models included age, GDS score, prior diarrhea, and AMAN on nerve conduction results.
Participant mean age was 57, and 57.1% were men, with median time from symptom onset to study inclusion of 4 days. In patients with CSF samples, elevated protein was seen in about 69% but did not correlate with serum or CSF NfL levels. The most common presentation of GBS was the typical sensorimotor variant (66%). Treatments included intravenous immunoglobulin alone (77.6%) or with plasma exchange (10.2%).
GBS patients with preceding diarrhea had higher sNfL compared with GBS patients who had preceding respiratory symptoms and those who had no preceding infection symptoms (134.90 versus 47.86 versus 38.02 pg/mL respectively, P=0.016). AMAN was associated with a higher sNfL level compared with all other categories (199.53 versus 46.77 pg/mL, P=0.006).
Cutoff levels for sNfL were identified for predictive values:
- Serum NfL < 34 pg/ mL predicted complete recovery, defined as the ability to run at 1 year (OR 6.59, 95% CI 2.02-21.46, P=0.002, specificity 82.1%, sensitivity 69.2%).
- Serum NfL >248 pg/mL predicted inability to run at 1 year (OR6.81, 95% CI 1.64-28.21, P=0.008, specificity 94.2%, sensitivity 39.3%).
- Serum NfL >319 pg/mL predicted inability to walk independently at 1 year (OR5.20, 95% CI 1.02-26.34, P=0.047, specificity 89.4%, sensitivity 33.3%).
The findings raise new questions, including use of sNfL for monitoring, the editorialist observed. “Such monitoring could be especially useful in patients with tetraparalysis, treatment-related fluctuations, and transition to chronic inflammatory demyelinating polyneuropathy,” Jacobs noted, in addition to a secondary outcome measure to evaluate new treatments.
“More extensive studies are required to decide if NfL truly adds to the existing clinical prognostic models in GBS,” he added. “The authors already defined cut-off values for NfL as a single predictor, but more likely in my view is that NfL will be combined with clinical features to reach most predictive power.”
Limitations of the study include the lack of exclusion criteria in the database. All patients with GBS and variants were included, without information about possible prior neurologic disorders.
-
Baseline serum neurofilament light (sNfL) levels were increased in patients with Guillain-Barré syndrome (GBS) and were an independent predictor of 1 year functional outcome, data from the ongoing prospective International GBS Outcome Study showed.
-
More extensive studies are required to decide whether NfL truly adds to existing clinical prognostic models in GBS, the editorialist noted.
Paul Smyth, MD, Contributing Writer, BreakingMED™
This work was supported by Fondo de Investigaciones Sanitarias (FIS), Instituto de Salud Carlos III, Spain and FEDER under grant FIS19/01407, personal grant Rio Hortega CM19/00042, personal grant SLT006/17/00131 of the Pla estratègic de recerca i innovació en salut (PERIS), Departament de Salut, Generalitat de Catalunya, and the ER20P3AC7624 project of the ACCI call of the CIBERER network, Madrid, Spain.
Querol has provided expert testimony for Grifols, Sanofi-Genzyme, Novartis, UCB, Roche, and CSL Behring and received research funds from Novartis Spain, Sanofi-Genzyme, and Grifols.
Jacobs declared no competing interests.
Cat ID: 130
Topic ID: 82,130,730,130,192,925



Create Post
Twitter/X Preview
Logout