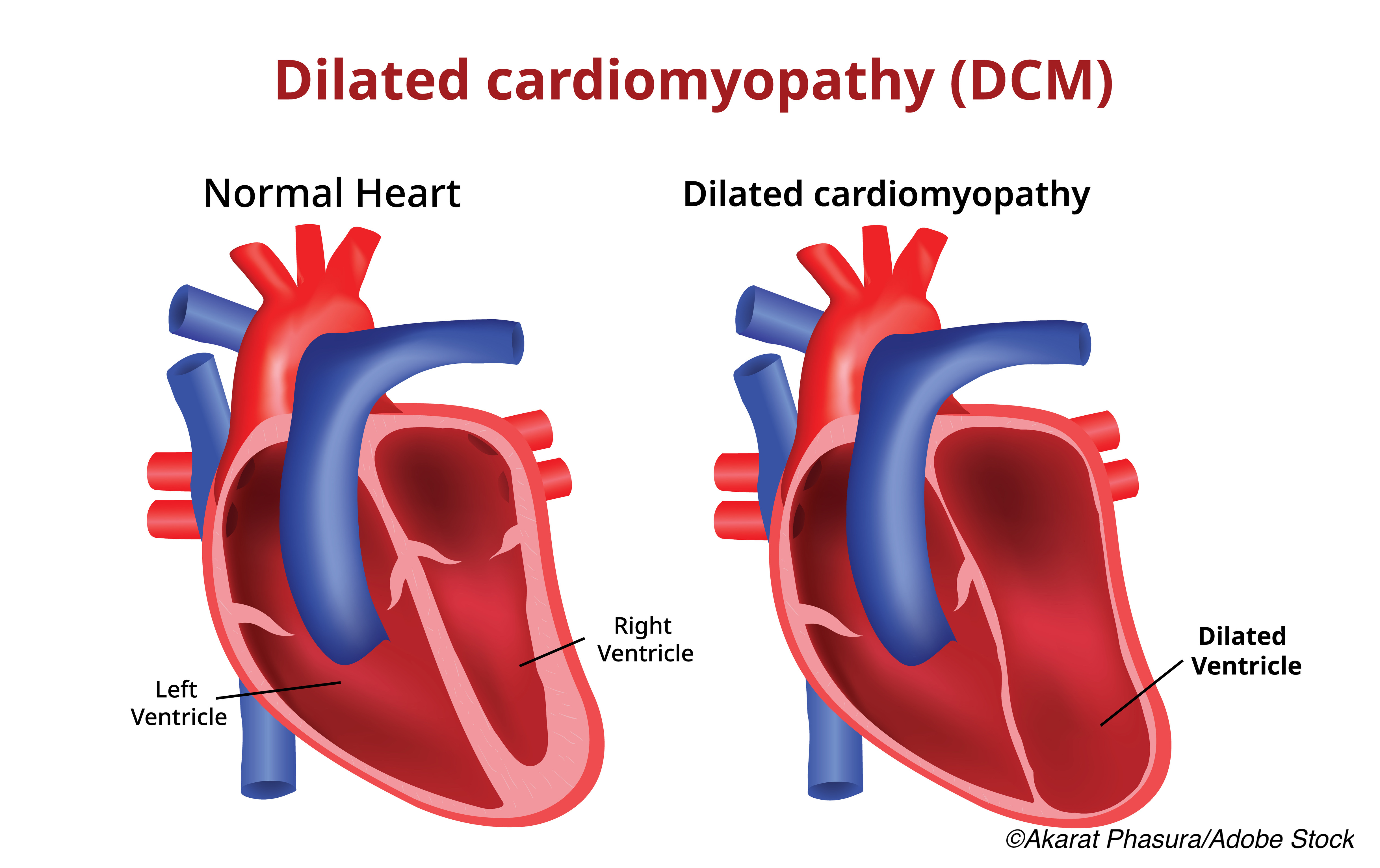
Identifying the genetic drivers of dilated cardiomyopathy (DCM)—which truncating variant is the patient carrying, the gene encoding filamin C (FLNCtv) or the one encoding TTN (TTNtv)—may be a more reliable way to assess true risk of sudden cardiac death or end-stage heart failure than simply relying on measurement of left ventricular function.
For example, a cohort study comparing 167 consecutive FLNCtv carriers to 244 TTNtv carriers, who were matched for left ventricular ejection fraction (LVEF) rates, found that the risk of developing a malignant ventricular arrhythmia (MVA) was greater in FLNCtv carriers than observed in TTNtv carriers regardless of baseline LVEF. The findings were published online in JAMA Cardiology.
“There was no difference in freedom from MVA between FLNCtv carriers with mild to moderate or severe (LVEF ≤35%) [left ventricular systolic dysfunction] (HR, 1.29 [95% CI, 0.45-3.72]; P=0.64). Carriers of FLNCtv with impaired LVEF at baseline evaluation (n=69) had reduced freedom from MVA compared with 244 TTNtv carriers with similar baseline LVEF (for mild to moderate LVSD): HR, 16.41 [95% CI, 3.45-78.11]; P<0.001; for severe LVSD: HR, 2.47 [95% CI, 1.04-5.87]; P=0.03),” wrote Mohammed Majid Akhtar, MD, of the Department of Inherited Cardiovascular Diseases, Bart’s Heart Centre St. Bartholomew’s Hospital, London, United Kingdom, and colleagues.
As a result, the authors suggest that FLNCtv carriers should be considered candidates for prophylactic implantable cardiovascular defibrillators at a higher LVEF value than the current standard, which is LVEF of ≤35%. In this study, “[P]atients who were FLNCtv carriers with mild to moderate LVSD or severe LVSD had significantly more arrhythmic end point events compared with patients who were TTNtv carriers with DCM, despite similar severities of LVSD.”
In an editorial that accompanied the study by Akhtar et al, Northwestern University Feinberg School of Medicine researchers Sadiya S. Khan, MD, MSc, and Jane E. Wilcox, MD, MSc, wrote that the study by Akhtar and colleagues was a much needed step in the right direction since it highlights the importance of genetics in diagnosis of DCM:
“Identification of the underlying mechanism in DCM is needed to support more accurate risk stratification for ICD therapy, beyond EF, which has limited sensitivity and specificity. Incorporation of genotyping will enable greater and much needed precision in classification of DCM subtypes that are associated with higher risk of ventricular arrhythmias (e.g., FLNCtv, LMNA, SCN5A, DES, and DSP),” they wrote. “In addition to arrhythmia risk, specific genetic variants may provide important diagnostic and prognostic information, which may guide individual physician-patient discussions.”
Already, Kahn and Wilcox noted, a number of societies—the American College of Cardiology, the American Heart Association, the Heart Failure Society of America, and the Heart Rhythm Society/European Heart Rhythm Association—are incorporating panel-based genetic testing into DCM guidelines.
The study by Akhtar and colleagues identified 167 individuals (55 probands from 61 families) who were being treated at 19 European centers to comprise the FLNCtv cohort and followed them for a median of 20 months. At baseline, the median age of probands was 46 and the median age of relatives was 41. The most common presenting symptom was dyspnea, followed by palpitations.
The FLNCtv probands were more likely to be men, to have had a history of isolated SCD, and were more likely to have a lower baseline LVEF compared with relatives (37.3% versus 57.2%).
The primary endpoint was a composite of an MVA event—defined as “sudden cardiac death, aborted sudden cardiac death, appropriate implantable cardioverter-defibrillator shock, and/or sustained ventricular tachycardia”—and end-stage heart failure (ESHF). The secondary endpoint was MVA events only.
“Twenty-nine patients (17.4%) reached the primary end point: MVA in 19 patients (66%) and ESHF in 10 patients (34%). The most frequent MVA end point was SCD (n=8), followed by aborted SCD (n=4), appropriate ICD shock (n=4), and sustained ventricular tachycardia (n=3; two of whom had appropriate antitachycardia pacing). The ESHF end points were most commonly HTx (n=9) followed by mortality associated with ESHF (n=1). The median duration from listing for advanced heart failure therapies to undergoing HTx was 76 days (IQR, 32-195 days).”
Comparing FLNCtv patients who had impaired LVEF at baseline to 244 TTNtv carriers who also had dilated cardiomyopathy and impaired LVEF, Akhtar and colleagues found the “composite primary end point of MVA or ESHF events was reach by 71 patients (47 of 244 [19.3%] TTNtv carriers vs 24 of 69 [34.8%] FLNCtv carriers; P<0.001]). The arrhythmic secondary end point was reached by 39 patients (24 of 244 [9.8%] TTNtv carriers vs 15 of 69 [21.7%] FLNCtv carriers; P<0.001]).”
Among the limitations noted by the authors was the lack of racial/ethnic diversity in the cohort, almost all of whom were White. Additionally, data were not uniformly collected.
-
In a cohort study of 167 consecutive FLNCtv carriers, 29 (17%) reached the primary end point of malignant ventricular arrhythmia (MVA) or end-stage heart failure (ESHF), and the risk of MVA or ESHF was greater among FLNCtv carriers than observed among TTNtv carriers.
-
The findings suggest that higher LVEF values than those currently recommended should be considered for a prophylactic implantable cardioverter-defibrillator in FLNCtv carriers.
Peggy Peck, Editor-in-Chief, BreakingMED™
Akhtar had no disclosures.
Khan reported receiving grants from the American Heart Association and the National Institutes of Health during the conduct of the study and outside of the submitted work.
Wilcox reported receiving consulting fees and honoraria from Amgen, Boerhinger Ingelheim, and Abbott and serves onthe scientific advisory board for Cytokinetics.
Cat ID: 914
Topic ID: 74,914,497,730,914,192,925



Create Post
Twitter/X Preview
Logout