Compared to standard therapy with enoxaparin, abelacimab, a novel anticoagulant that targets factor XI with the goal of hemostasis-sparing anticoagulation, demonstrated significantly greater reductions of venous thromboembolism (VTE) following total knee arthroplasty, researchers reported at the virtual congress of the International Society on Thrombosis and Hemostasis (ISTH), in Philadelphia.
In the phase II trial, low-dose abelacimab (30 mg IV) was non-inferior to enoxaparin 40 mg IV, and at 75 mg abelacimab achieved statistically significant superior results (P<0.001), wrote Peter Verhomme, MD, of the Department of Cardiovascular Sciences, Vascular Medicine, and Hemostasis, Katholieke Universiteit Leuven, Leuven, Belgium, and co-investigators for the ANT-005 TKA trial in a simultaneous publication in The New England Journal of Medicine.
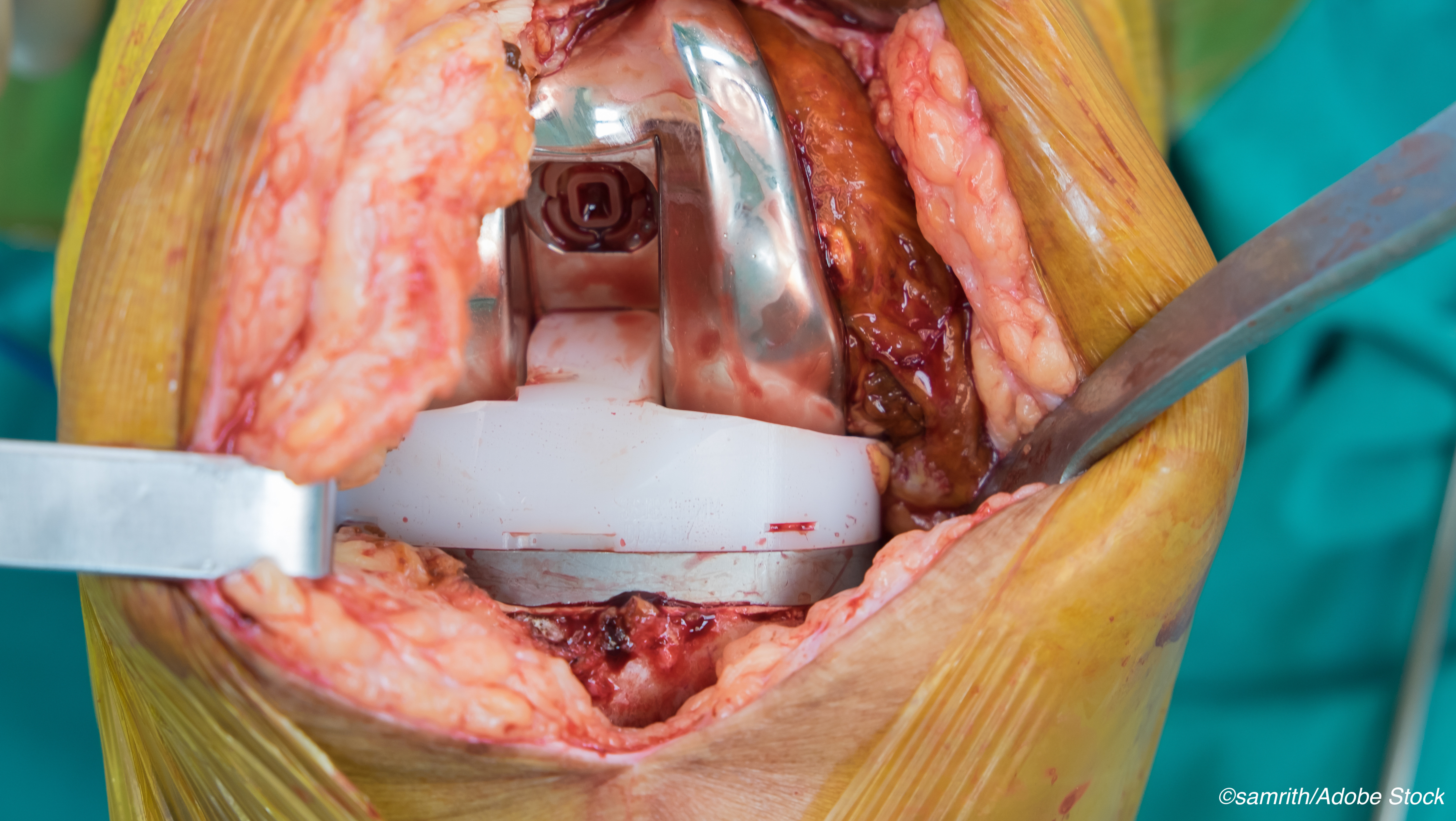
The open-label, parallel-group trial enrolled 412 patients undergoing total knee replacement. The patients were randomly assigned to 30 mg, 75 mg, or 150 mg abelacimab in a single IV dose postoperatively. The comparator group received 40 mg enoxaparin subcutaneously daily. “The primary efficacy outcome was venous thromboembolism, detected by mandatory venography of the leg involved in the operation or objective confirmation of symptomatic events. The principal safety outcome was a composite of major or clinically relevant nonmajor bleeding up to 30 days after surgery.”
Abelacimab is a fully human monoclonal antibody capable of locking Factor XI into an inactive precursor thus preventing XI from activating factor XIIa or thrombin.
The researchers evaluated VTE using venograms.
Among the results:
- VTE occurred in 13 of 102 patients in the 30 mg abelacimab group.
- VTE occurred in 5 of 99 patients in the 75 mg abelacimab group.
- VRE occurred in 4 of 0f 98 patients in the 150 mg abelacimab group.
Among the 101 patients in the enoxaparin group, 22 developed VTE.
“All three abelacimab regimens met the criterion for noninferiority to enoxaparin. The difference in risk (abelacimab minus enoxaparin) with the 30-mg abelacimab regimen was −9.2 percentage points (95% confidence interval [CI], −19.4 to 1.1; P=0.08 for superiority), whereas the difference with the 75-mg abelacimab regimen was −16.8 percentage points (95% CI, −26.0 to −7.6; P<0.001 for superiority) and the difference with the 150-mg abelacimab regimen was −17.8 percentage points (95% CI, −26.7 to −8.8; P<0.001 for superiority),” the study authors found. “The per-protocol analysis yielded similar results.”
Looking at hemostasis, there were no clinically relevant bleeding events among patients treated with enoxaparin, compared to 2% in each of the abelacimab groups.
“Serious adverse events occurred during the trial intervention in 1%, 3%, and 1% of the patients in the 30-mg, 75-mg, and 150-mg abelacimab groups, respectively, and in none of the patients in the enoxaparin group. None of the abelacimab infusions were stopped early because of hypersensitivity reactions, and no antidrug antibodies were detected with abelacimab infusion,” they wrote.
The researchers attributed the lower rate of thrombosis among abelacimab patients compared with enoxaparin-treated patients to the novel agents unique mechanism of action, which highlights “the role of factor XI in the pathogenesis of venous thrombosis after surgery. Factor XI can be activated by factor XIIa or by thrombin and is important for thrombus growth and stabilization. Abelacimab inhibits the activation of factor XI by either activator; the findings in this trial suggest that factor XI is at least as important as tissue factor in the pathogenesis of postoperative venous thromboembolism. Therefore, factor XI is an attractive target for thromboprophylaxis. Additional studies are needed to determine the efficacy of this mechanism of factor XI inhibition for the treatment of established venous or arterial thrombosis.”
But the researchers also had words of caution about their results. For example, the low bleeding rates may be due to the small sample size, rather than the effect of abelacimab. Also, 2% of patients did not have venogram analysis, although that 2% was spread across all treatment groups. Moreover, recruitment to the trial was stopped early for administrative reasons, but the researchers said that the halt did not affect the efficacy assessment.
They concluded that more studies are needed to “…determine whether anticoagulant strategies targeting factor XI can dissociate thrombosis from hemostasis.”
-
Be aware that this report discusses a drug that is not yet approved for clinical use.
-
In dose-finding parallel trials comparing abelicimab to standard enoxaparin therapy, abelicimab at any dose was non-inferior to enoxaparin and at 75 mg and 150 mg doses and it was superior to standard enoxaparin in preventing VTE post total knee athroplasty.
Peggy Peck, Editor-in-Chief, BreakingMED™
The study was funded by Anthos Therapeutics.
Verhomme reported a consultant agreement with Anthos, various grant support, data and safety monitority, lecture free and other contact agreements with Bayer Healthcare, Hoehringer Ingelheim, Bristol-Myers Squibb, Daichi Sankyo Company, LEO Pharma AS, Pfizer, and Portola Pharmaceuticals.
Cat ID: 309
Topic ID: 74,309,730,309,914,118,192,925



Create Post
Twitter/X Preview
Logout