In the largest randomized trial of asymptomatic patients with severe carotid artery stenosis to date, there was no long term difference in outcomes between carotid endarterectomy (CAE) or carotid artery stenting (CAS), according to results from the ACST-2 trial.
The findings from the 3,625-patient trial, which was conducted at 130 centers in 33 countries—most of them in Europe—were reported in a Hot Line presentation at the ESC 2021 Congress The Digital Experience and simultaneously published online by The Lancet.
At 5 years post-procedure, “1% had disabling stroke or death procedurally (15 allocated to CAS and 18 to CEA) and 2% had non-disabling procedural stroke (48 allocated to CAS and 29 to CEA),” said principal investigator Alison Halliday, MD, of the University of Oxford, U.K. She explained that excess non-disabling strokes in the CEA arm were mostly Rankin Scale score 0, meaning “that at 6 months they had no stroke symptoms.”
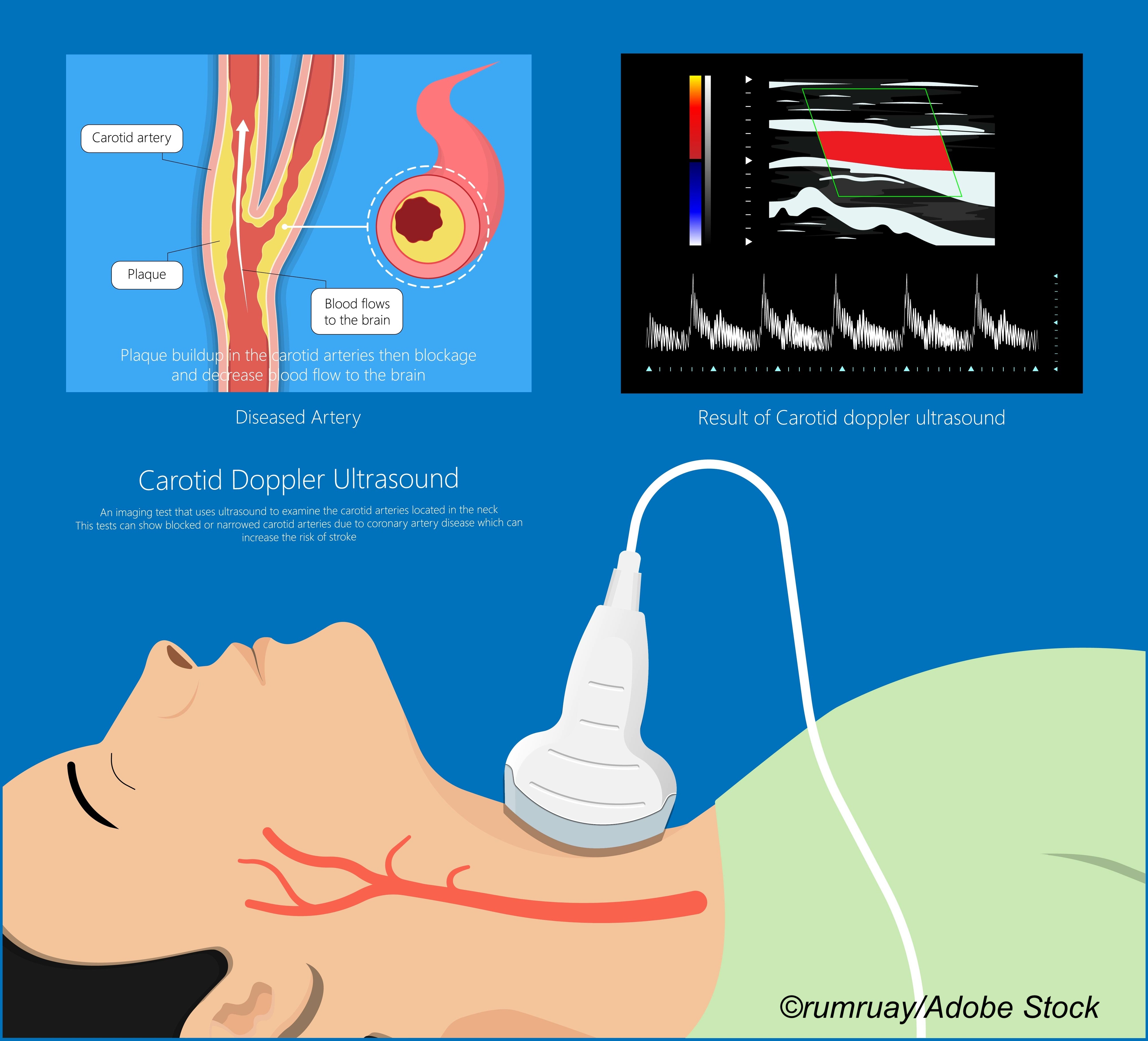
Patients were enrolled over a 12-year period spanning from Jan. 15, 2008, through Dec. 31, 2020. Entry criteria included “severe unilateral or bilateral carotid artery stenosis (generally 60% or higher on ultrasound); this had not caused any relevant neurological symptoms in the preceding 6 months; there was CT or MRI confirmation of suitability for CAS and for CEA (which would also have been used to exclude from trial entry any patient without sufficient stenosis to justify intervention); the doctor and patient agreed that a carotid procedure should be undertaken, but they were substantially uncertain whether this should be CAS or CEA.”
“We have shown that, for patients with a severely narrowed carotid artery, stenting and surgery have similar effect on the chances of having a disabling or fatal stroke. The risk from each procedure is about 1%. After that, however, the annual risk over the next five or more years is halved, from 1% down to 0.5% per year,” Halliday said.
During the Hot Line panel discussion, several audience members asked about medical therapy rather than an intervention. Halliday explained that the trial only enrolled patients for whom the clinical decision was that CAS or CAE was the best clinical option, clarifying that “they just had not decided which option they preferred.”
Halliday discussed the findings during an ESC press briefing prior to the Hot Line presentation, and BreakingMED asked her which procedure she would choose if she had a carotid stenosis that required intervention. “Well, I am a surgeon, so I have to say that is my bias,” Halliday said. “But, really it would depend upon the lesion: if it were very calcified or very tortuous, those would be factors.” That said, she added that the experience of the operators—surgeon or interventionalist—as well as the experience of the center—low versus high volume—would be also be factors in selecting the type of revascularization.
Hot Line discussant Marco Roffi, MD, of the University Hospital of Geneva, an interventional cardiologist, said a likely explanation for the high rate of non-disabling strokes seen in the CAS arm may reflect changing technology—better stents, better procedures—over the course of the trial. Moroever, the difference “was mainly driven by strokes with a Rankin disability score of zero, meaning that at 6 months there were no symptoms at all from the stroke.”
In terms of limitations, Roffi noted “there was a sample size reduction over time—Initially planned for 5,000 patients, with 3,625 patient limiting the statistical power. The enrollment went over a very long period of time, and this may have introduced confounders such as changes in equipment technique and pharmacological therapy. Likely many centers enrolled few patients, raising the concern of a low volume operator, and low volume centers. Indeed, if somebody would assume that all the centers started enrolling at the same time, which obviously is not correct, the average enrollment per center would have been of two patients per year. And, finally, from the website we know that 80% of the center’s enrolled 39% of the patients, so information on credentialing and experience of the interventions was limited.”
Another limitation, “was a lack of systematic myocardial infarction assessment,” he added.
Limitations aside, Roffi concurred with Halliday’s conclusions: “Ladies and gentlemen, this was the largest carotid artery stenting versus endarterectomy trial conducted in asymptomatic patients, and it showed no difference in procedural events with the exact exception of an excess of minor non-disabling strokes, which were asymptomatic. After extending out, there was no difference in stroke rates beyond 30 days up to five years. So, my take on ASCT-2 is that, with documented expertise, carotid artery stenting should be offered as an alternative to carotid endarterectomy in patients with asymptomatic carotid stenosis and suitable anatomy.”
If there are no anatomical barriers, the key considerations in deciding whether to open a blocked carotid with a stent or with surgery is the expertise of the operators, said T. Sloane Guy, MD, professor of surgery at Thomas Jefferson University Sidney Kimmel Medical College in Philadelphia.
Guy, who is a member of the American College of Cardiology’s Cardiac Surgery Team Council, discussed the ACST-2 results with BreakingMED in a telephone interview.
“Purely from a medical point, not from what the patient might like to do, there are a number of factors that should determine the best option. One is anatomic, what you see on imaging. Because I do heart surgery, I look at it a little differently, say, than a vascular surgeon, and the reason why is that we, as cardiac surgeons, we are very used to a collaborative decisions,” Guy said. “In fact just 15 minutes ago, I was discussing a case that could be done either open surgery, or with a catheter based procedure, a similar sort of scenario… And so, basically, what we were doing is we were deciding together in a collaborative way, which was best for this particular patient, given their anatomy and given their surgical risk, and the pros and cons, and then we decided that we’re going to do surgery on the patient, that that would be better for this patient.”
The patients in ACST-2 were asymptomatic, and Guy pointed out that in asymptomatic patients a carotid blockage—in this study it had be at least 60%—is likely to be picked up by the presence of bruits during a clinical examination by a primary care provider or by an imaging study, which means that clinician will be making a referral. The considerations about where to refer should take into account the availability of both surgical and catheter-based interventions, Guy explained.
The ASCT-2 findings are “based on idealized patients and top operators,” Guy said. “I’m unique, in that I’ve been a general practitioner doctor and I’ve actually been in that position. I think it’s important for family practice physicians or even a general cardiologist to understand if you send a patient to someone who can only do surgery or catheter-based procedures, that is what the patient will be offered. What I want to do is I want to refer this patient to a team with expertise in surgery and catheter-based procedures. And sometimes, the solution will be both—we do an endarterectomy and then use a stent if the lesion extends high up. I want the best possible thing for the patient.”
-
ACST-2 found that, among asymptomatic patients, carotid artery stenting (CAS) provided similar results in terms of benefit and safety as carotid endarterectomy (CEA).
-
The ACST-2 trial provides evidence that CAS and CEA carry similar risks and provide comparable benefit, but it remains unknown if such interventions are needed in the presence of optimal medical therapy.
Peggy Peck, Editor-in-Chief, BreakingMED™
ACST-2 is currently funded from the core support from the Medical Research Council(MRC), the British Heart Foundation, and Cancer Research UK for the University of Oxford’s NDPH. The trial had grants from the BUPA Foundation (BUPAF/33a/05) and National Institute for Health Research Health Technology Assessment programme (HTA06/301/233) until 2013.
Halliday had no disclosures.
Roffi disclosed institutional support from Teruma and Biotronik.
Guy had no disclosures.
Cat ID: 130
Topic ID: 82,130,730,204,745,8,130,38,748,192,925,159,493,203