When a person is infected by SARS CoV-2—the pathogen that causes Covid-19 disease—the effects on body organs is pervasive, including impairing the normal functioning of the pancreas so that less insulin is produced, presenting a possible link to onset of diabetes among pandemic patients, researchers reported at the 2021 virtual meeting of the European Association for the Study of Diabetes.
In a special session devoted to Covid-19’s impact on the pancreas, Shuibing Chen, MD, of Weill Cornell Medicine, New York, said, “Covid-19 represents a wide range of systemic problems. In addition to respiratory failure, many individuals with Covid-19 present with multi-organ clinical complications, including cardiac defects, gastrointestinal symptoms, kidney damage, abnormal liver function, neurological manifestations, and a number of metabolic abnormalities. Thus, there is strong need to develop a method to systematically study the impact of SARS-CoV-2 infection on different host tissues.”
She described her work using human pluripotent stem cells and organoids—clusters of types of cells in lab conditions that mimic the function of a particular organ—to systematically evaluate the processes and cellular response during viral infection and also screen for possible drugs to prevent infection.
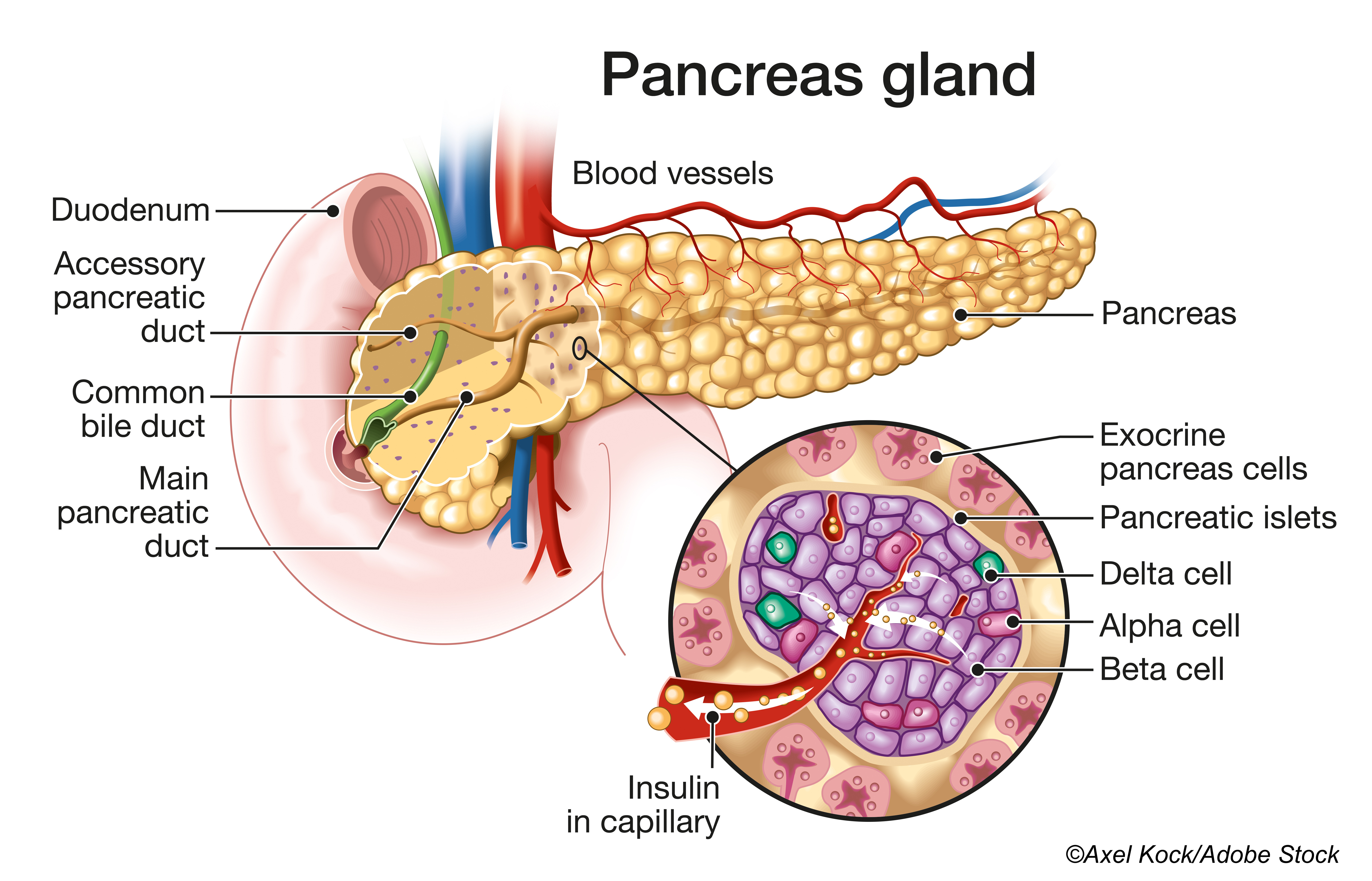
“By screening 10 different type of cells and organoids, we found that lung, colon, heart, liver, and pancreatic organoids and dopamine neurons can be infected by SARS-CoV-2,” Chen said. “This work presented the first stem cell model to understand which organs and cells within those organs can be infected by SARS-CoV-2, which in turn led to a clinical trial to study beta cell function in Covid-19 patients. Work on this study is continuing,” she explained.
Chen and colleagues reported the first organoid-based screening study and identified several drug candidates blocking SARS-CoV-2 entry into host cells.
In addition, they performed single-cell RNA-sequencing and confirmed that multiple types of islet cells in the pancreas were susceptible to SARS-CoV-2. Upon SARS-CoV-2 infection, beta cells produced less insulin and more alpha and acinar cell markers. The cells still make insulin, but infection meant the level of insulin they make is much lower. At the same time, the infected beta cells also produce glucose and digestive enzymes, suggesting the virus has the ability to fundamentally change cellular fate.
She said there have been case reports of new onset diabetes several weeks after Covid-19 infection. “It is definitely worth investigating the rate of new onset diabetes patients in this Covid-19 pandemic,” Chen said.
“Organoids can be used as a powerful model to study the potential of a virus to infect, the host response, immune cell-mediated host damage and, finally, for drug screening,” she said. Her researcher team is working to develop multi-cellular organoid models and humanized animal models, which more accurately replicate the development of disease in individual patients, and applying these models to develop new anti-viral drugs.
In another study discussed at the symposium, Francesco Dotta, MD, of Università degli Studi di Siena, Italy, said, “The SARS-CoV-2 virus attacks specific host tissues because of the presence of viral receptors on the surface of the target cells. As such, virus binding to the angiotensin-converting enzyme-2 (ACE2) protein is the key determinant for its entry, propagation and transmissibility.”
He and colleagues at the University of Pisa, University of Leuven and University of Brussels determined that ACE2 was expressed in human pancreatic islet cells, where it is preferentially expressed in insulin producing beta-cells. “We also demonstrated that ACE2 levels were increased under pro-inflammatory conditions, thus confirming the link between inflammation and ACE2 also in pancreatic islet beta cells,” he said.
In commenting on the study, Francesco Rubino, MD, of King’s College London, told BreakingMED that the studies appear to have strong theoretical backbones, but more study will be required before the results can be translated to the clinic.
“The researchers were able to show that the virus does appear to have an affinity for pancreatic cells,” Rubino said. “It also appears that this infection does cause dysfunction in these cells. Both studies show there is a plausible biological link between Covid-19 and diabetes, which we and others have noted in our clinical observations.”
However, he suggested that the studies still have not shown a definitive link to development of diabetes through the infection and inflammation that is created in the pancreas. “But if you put these studies and observations together, this does seem to be a reasonable scientific theory,” Rubino said.
He said researchers in Europe are putting together a database of hundreds of cases of patients with Covid-19 and diabetes in hopes of teasing out causes and effects.
While the studies’ researchers have suggested that anti-IL6 and other drugs might be useful in combating Covid-19 impact on the pancreas and diabetes, Rubino said the work is too early to make any treatment recommendations.
-
Covid-19 can infect the pancreas and cause inflammatory damage in insulin-producing cells.
-
The laboratory work hints that some drugs could be effective in treating Covid-19 related disease, but additional studies are needed before any recommendations can be made.
Edward Susman, Contributing Writer, BreakingMED™
Chen and Dotta disclosed no relationships with industry.
Rubino disclosed relationships with Medtronic, Novartis and Johnson & Johnson.
Cat ID: 412
Topic ID: 98,412,728,791,932,730,933,12,13,413,926,192,412