The calcium sensitizer levosimendan was no better than placebo in changing decline in supine slow vital capacity (SVC) for patients with amyotrophic lateral sclerosis (ALS) in the phase III REFALS trial.
Change from baseline in supine SVC at 12 weeks, the primary endpoint, was –6.73% with levosimendan and –6.99% with placebo, with a nonsignificant estimated treatment difference (0.26%, 95% CI –2.03 to 2.55, P=0.83), reported Merit Cudkowicz, MD, of Massachusetts General Hospital in Boston, and co-authors in Lancet Neurology.
“Levosimendan was not superior to placebo in maintaining respiratory function in a broad population with ALS,” they wrote. “Although levosimendan was generally well tolerated, increased heart rate and headache occurred more frequently with levosimendan than with placebo. The possibility of a clinically relevant subgroup of responsive individuals requires further evaluation.”
The group conducted a double-blind study that included patients from 99 specialist centers in 14 countries. All were 18 or older with probable or definite ALS per El Escorial revised criteria. All had sitting SVC of 60-90% of predicted normal value (mean sitting SVC 76.5% of predicted) and were able to swallow the oral medication.
Mean age overall was about 59, and 38% were women. Disease onset was spinal in 81% and bulbar in 19%. The mean duration of ALS symptoms (symptom onset to randomization) was 25.9 months.
The use of tirasemtiv, reldesemtiv, and botulinum toxin was prohibited during the trial, and participants already receiving riluzole or edaravone could continue on stable dosing, though starting these medications during the trial was prohibited. Patients on assisted ventilation or using a diaphragm pacing system within 3 months before screening were excluded. “These criteria would define a population with some respiratory decline but not yet in need of ventilatory support,” the researchers noted.
Participants were randomized to either levosimendan titrated to 1 mg orally twice daily (n=329) or placebo (n=167) between June 2018 and June 2019. Follow-up was between June 2018 and June 2020, with median follow-up of 50.1 weeks. Median duration of treatment was 47.9 weeks.
A secondary endpoint at the 48-week conclusion of the trial—a combined assessment of function and survival, a rank score based on change in the revised Amyotrophic Lateral Sclerosis Functional Rating Scale adjusted for survival time—did not differ between levosimendan and placebo.
The most frequent adverse events for levosimendan and placebo, respectively, were increased heart rate (33% versus 7%), falling (26% versus 29%); headache (29% versus 22%), and dyspnea (18% versus 19%). There were 33 deaths in the levosimendan group and 20 in the placebo group. Treatment was stopped by 41% of the levosimendan group and 37% of the placebo group, mostly due to adverse events or progressive disease.
“When designing the REFALS study, in their sample size calculation, Cudkowicz and colleagues proposed a small difference between the study groups as clinically significant (3.6%),” noted Mamede de Carvalho, MD, and Michael Swash, MD, both of the University of Lisbon, Portugal, in an accompanying editorial. “Considering this small effect, and that the trial did not meet any of the prespecified endpoints, levosimendan is probably ineffective in ALS.”
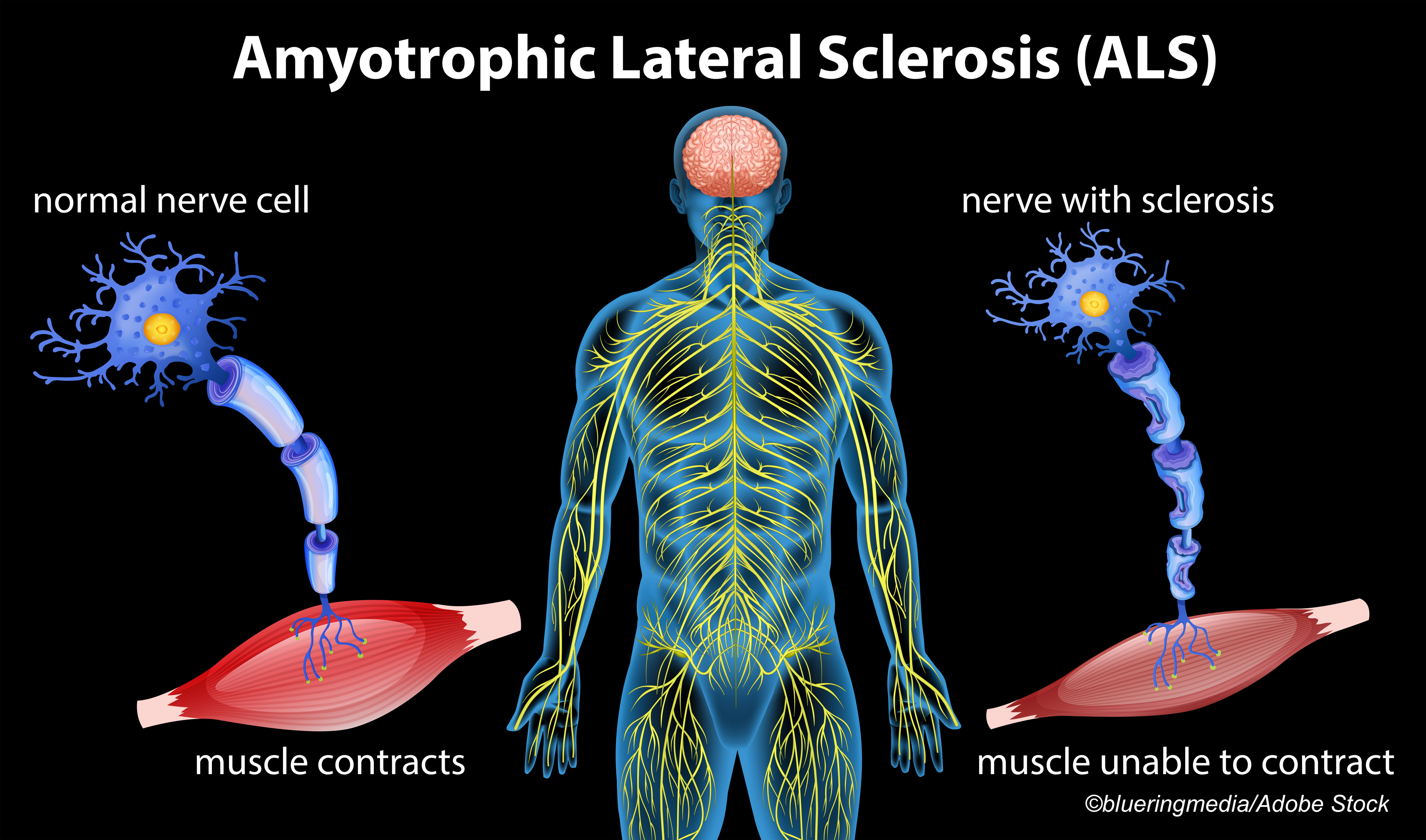
“Muscle cell physiology is different in skeletal muscles and the myocardium,” de Carvalho and Swash added. While levosimendan had some positive effects in the diaphragm of healthy controls in other research, “its effect on partly denervated skeletal muscle is unknown. Therefore, the results of the REFALS study should not necessarily prevent testing of other drugs with a similar mechanism of action, such as reldesemtiv.”
Calcium sensitizers have been studied extensively in the setting of heart failure: troponin C in cardiac muscles initiates muscle contraction in a calcium-dependent manner and levosimendan increases the calcium sensitivity of troponin C in cardiac muscle and slow twitch skeletal muscles. An intravenous form is approved in Europe for severe heart failure, but not in the U.S.
In ALS, the phase II LEVALS trial found that levosimendan did not improve sitting slow vital capacity, though 2-week supine SVC was superior to placebo. Adverse effects included headache (29%) and tachycardia (19%) on the 1 mg twice daily dose.
“The significant differences favoring levosimendan over placebo in supine SVC after 14 days of treatment identified in post-hoc analyses of the LEVALS phase II trial were not replicated in the current trial,” Cudkowicz and colleagues noted. “These findings suggest that positive effects from phase II trials should be interpreted with caution when designing a phase III trial.”
A REFALS extension study has been completed and a separate report is planned.
Limitations of the REFALS trial included a lack of run-in period and the absence of upright vital capacity assessment.
There remains a huge need for novel pharmaceutical options to treat ALS, Cudkowicz and co-authors observed. “Although levosimendan does not appear to be useful in a broad population with amyotrophic lateral sclerosis, the possibility of a clinically relevant subgroup of responsive individuals with a short duration of disease, worse respiratory function at baseline, and faster progression of the disease should be further evaluated,” they wrote.
-
In the phase III REFALS trial, levosimendan was not superior to placebo in maintaining respiratory function in a broad population with ALS.
-
Whether there’s a subgroup of responsive ALS patients should be evaluated, the researchers suggested.
Paul Smyth, MD, Contributing Writer, BreakingMED™
This study was funded by the Orion Corporation.
Cudkowicz reported consultancy fees from Biohaven Pharmaceuticals, Eli Lilly, Orion Corporation, Revelescio, Wave Pharmaceuticals, Mitsubishi Tanabe Pharma, Anelixis, Aclipse, Cytokinetics, Avexis, Sunovian, Disarm, ALS Pharmaceuticals, RRD, Biogen, and Takeda.
de Carvalho and Swash declared no competing interests.
Cat ID: 130
Topic ID: 82,130,730,130,192,925