In patients with severe mitral regurgitation (MR), transcatheter mitral valve replacement (TMVR) had positive effects on the severity of MR, reduced hospitalization for heart failure, and led to improved symptoms and quality of life at two years, according to a recent study published in the Journal of the American College of Cardiology.
“Severe, symptomatic mitral regurgitation (MR) is associated with a high morbidity and mortality. This is particularly true of secondary (or functional) MR with left ventricular (LV) dysfunction and heart failure, but also applies to primary (or degenerative) MR. Although medical therapies, such as beta-blockers and inhibitors of the renin-angiotensin-aldosterone pathways, have been associated with reverse LV remodeling and in some cases a reduction in the severity of MR, the outlook for patients with persistent severe MR remains poor. For these patients, surgical valve repair or replacement is an established option with recently updated recommendations to guide management decisions,” wrote David W. M. Muller, MBBS, MD, of St. Vincent’s Hospital Sydney, New South Wales, Australia, and colleagues.
Although TMVR is an option in selected patients with severe MR who are poor candidates for valve surgery, the intermediate- and long-term outcomes with TMVR have not been assessed. Muller and colleagues undertook this study, therefore, to assess the safety and efficacy of TMVR in severe MR patients in whom surgical repair carried a high risk.
They included the first 100 patients (mean age: 74.7 years, 69.0% men) enrolled in the non-randomized, prospective, global Expanded Clinical Study of the Tendyne Mitral Valve System, who were followed for two years. All patients had symptomatic grade 3+ or 4+ MR that was secondary or mixed (89.0%).
In all, 38.0% of patients had diabetes, 35.0% had atrial fibrillation, 74.0% had coronary artery disease, 47% had previous coronary bypass graft surgery, and 14% had previous stroke or transient ischemic attack. Ten percent had biventricular pacemakers and 23% had implantable cardioverter-defibrillators. In addition, 93.0% had MR of severity grade 4+, and 6.0% had grade 3+. Baseline left ventricular ejection fraction was a mean of 46.2, and all patients were symptomatic (62.0% NYHA functional class III; 4.0% NYHA functional class IV).
Patients underwent TMVR, which was done through a left anterolateral thoracotomy under general anesthesia.
“The valve prosthesis was delivered through a 36-F transapical sheath and attached to an epicardial pad using a braided, high-molecular-weight polyethylene tether. The length of the tether was adjusted to optimize seating of the prosthesis, and to minimize the risk of device displacement and paravalvular leakage. Patients were anticoagulated postoperatively for a minimum of three months using warfarin with a target international normalized ratio of 2.5 to 3.5,” researchers explained.
Implantation was successful in 97.0% of patients, with no intraprocedural deaths but six deaths before hospital discharge. At two years, nine patients withdrew from the study, 39 had died, and three missed follow-up visits, leaving 49 patients to complete the two-year follow-up.
At two years, all-cause mortality was 39.0%, with most deaths (43.6%) occurring in the first 90 days. The primary cause of death during the first 90 days was refractory heart failure in 11 patients and fatal arrhythmias in five.
At this same timepoint, 37 patients required hospitalization for heart failure, with 21 occurring in the first 90 days and 24 between 90 days and two years. During this time, the rate of heart failure hospitalization was reduced, from 1.30 events/year before the procedure to 0.51 events/year (P˂0.0001). In addition, 93.2% had no MR at this timepoint, and no patient had greater than 1+ MR.
Major adverse events included disabling stroke (five patients), and device related thrombus (one patient). Major, extensive, life-threatening, or fatal bleeds occurred in 27 patients. Device-specific adverse events included paravalvular leaks in nine patients, and the need for mitral valve reintervention in five patients. Two episodes of endocarditis occurred, with three additional cases of infective endocarditis. Thrombus occurred in six patients, all within the first six months post-op.
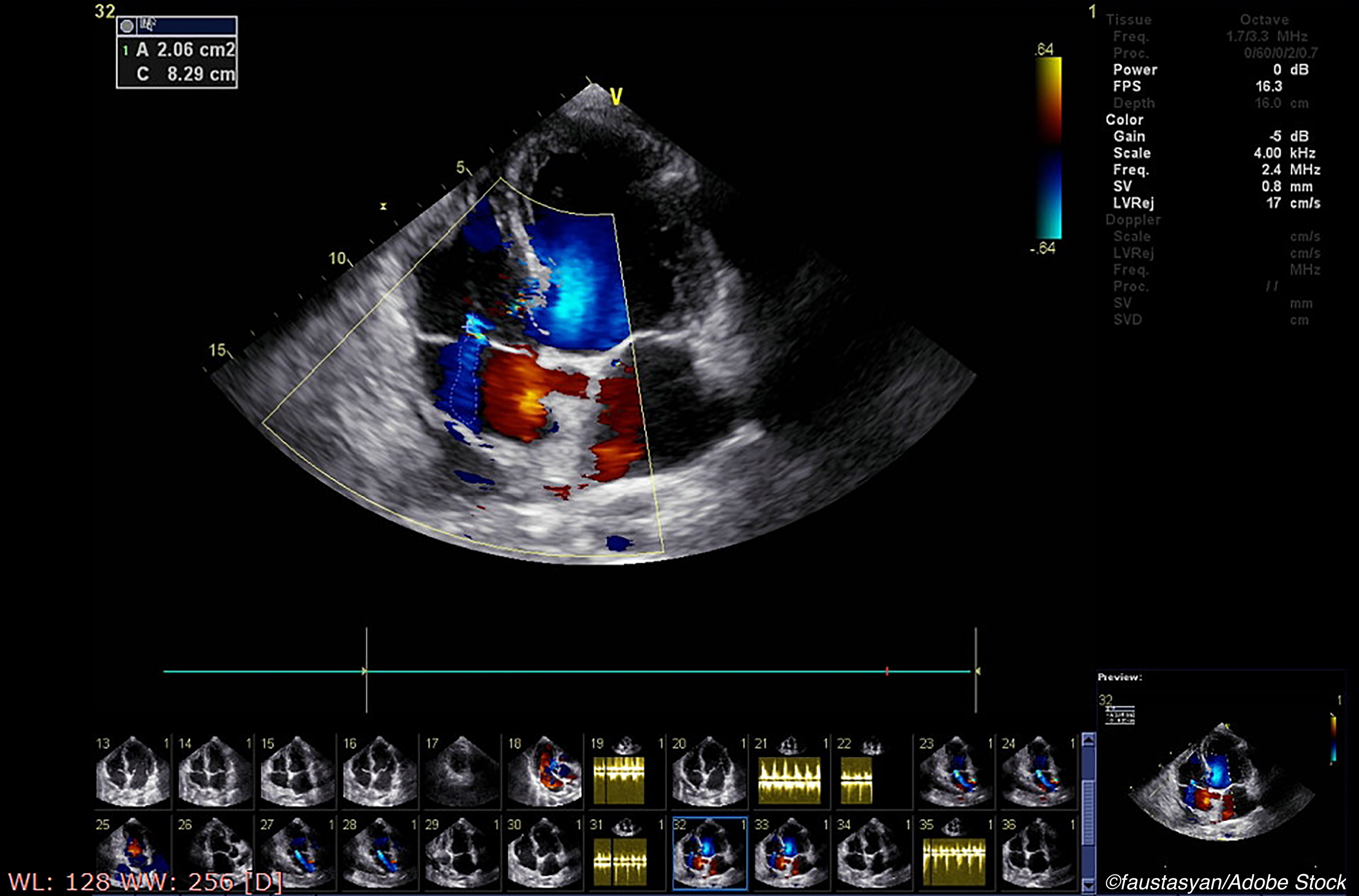
Forty-four patients underwent transthoracic echocardiographic imaging, and, “[w]hereas 99.0% of patients had MR grade 3+ or 4+ at baseline, 41 (93.2%) patients had no MR at 2 years, and the remaining 3 (6.8%) patients had mild (1+) MR. No patient had greater than grade 1+ MR at two-year follow-up,” noted Muller and colleagues.
In survivors, baseline left ventricular ejection (LVEF) was 45.6%, and this improved to 39.8% at two years (P=0.0012). Estimated right ventricular systolic pressure decreased from 47.6 mmHg to 32.5 mmHg (P<0.005).
At one year, 88.5% of patients were of NYHA functional class I or II, and this was sustained to two years in 81.6%. Baseline 6-minute walk distance was 244.8 m, and improved to 287.5 m at two years (P=0.46), while overall Kansas City Cardiomyopathy Questionnaire scores increased from 49.0 points at baseline to 67.2 points at two years (P<0.0001). A full 58.7% of patients had increases of greater than 5 points, and 56.5%, increases of greater than 10 points.
“The results on prosthetic valve function at two-year follow-up were reassuring. There were no cases of valve structural degeneration, no patient exhibited MR >1+, and transvalvular gradients remained low and stable during the study period. Despite these positive results, a possible competitive risk effect cannot be ruled out, especially considering that only 44 of 100 patients had an echocardiographic evaluation two years after valve implantation,” wrote Josep Rodés-Cabau, MD, PhD, of the Quebec Heart & Lung Institute, Laval University, Quebec City, Canada, and co-authors Ander Regueiro, MD, PhD, Michael J. Mack, MD, in an accompanying editorial.
They also noted that although roughly one-fourth of patients had major or life-threatening bleeding episodes, only 4% were related to the procedure or device.
Rodés-Cabau and colleagues concluded: “…the work from Muller et al provides important additional information to the emerging TMVR field. Although the data on two-year valve performance are reassuring, the results on clinical outcomes highlight the importance of both improving patient selection and follow-up, and determining the best antithrombotic strategy in these patients. Future efforts should also focus on ensuring longer-term clinical and echocardiography data availability. All these aspects will be important to accurately define the role of TMVR as an interventional alternative in the management of patients with MR, and should determine the role of this technology in a field where surgical repair/replacement and TEER are well-established therapies.”
Study limitations include its small size, the inclusion of consecutive patients treated during enrollment with no run-in phase, lack of echocardiograms from all time points in all patients, and lack of a clear perioperative management plan. Rodés-Cabau and colleagues adding that the greater than 10% of patients who were lost to follow-up was another important study limitation.
-
Reduced mitral regurgitation (MR) and hospitalizations for heart failure were seen after transcatheter mitral valve replacement (TMVR) over two years in selected patients with severe MR.
-
In these patients with MR who were at high risk for poor surgical outcome, TMVR also improved functional status and quality of life
Liz Meszaros, Deputy Managing Editor, BreakingMED™
The present paper is an analysis of the first 100 patients treated in the Expanded Clinical Study of the Tendyne Mitral Valve System supported by Abbott.
Muller has served as a consultant for Medtronic, Abbott, and Edwards Lifesciences; and has received research grant support from Abbott and Medtronic.
Rodés-Cabau has received institutional research grants from Edwards Lifesciences and Medtronic; and holds the Research Chair “Fondation Famille Jacques Larivière” for the Development of Structural Heart Disease Interventions.
Mack has served as the co-principal investigator or study chair for clinical trials sponsored by Abbott, Edwards Lifesciences, and Medtronic.
Regueiro reported no disclosures.
Cat ID: 306
Topic ID: 74,306,730,306,914,192,925