Chlorthalidone brought about better blood pressure (BP) control at 12 weeks compared with placebo in patients with advanced chronic kidney disease and inadequately controlled hypertension, according to a study published in The New England Journal of Medicine.
“Chlorthalidone, a thiazide-like diuretic, reduces cardiovascular morbidity, such as the incidence of stroke and heart failure, and cardiovascular mortality. However, its efficacy and safety among patients with advanced chronic kidney disease remain poorly understood. Several studies suggest that these drugs might be effective for treating hypertension in patients with chronic kidney disease,” explained Rajiv Agarwal, MD, of the Indiana University School of Medicine, and the Richard L. Roudebush Veterans Affairs Medical Center, Indianapolis, and colleagues.
“On the basis of preliminary evidence of an effect on blood pressure in patients with chronic kidney disease, we hypothesized that among patients with advanced chronic kidney disease and uncontrolled hypertension, chlorthalidone would decrease the 24-hour ambulatory systolic blood pressure. We also hypothesized that chlorthalidone would reduce the degree of albuminuria over 12 weeks and provide preliminary evidence that chlorthalidone is renoprotective and cardioprotective,” they added.
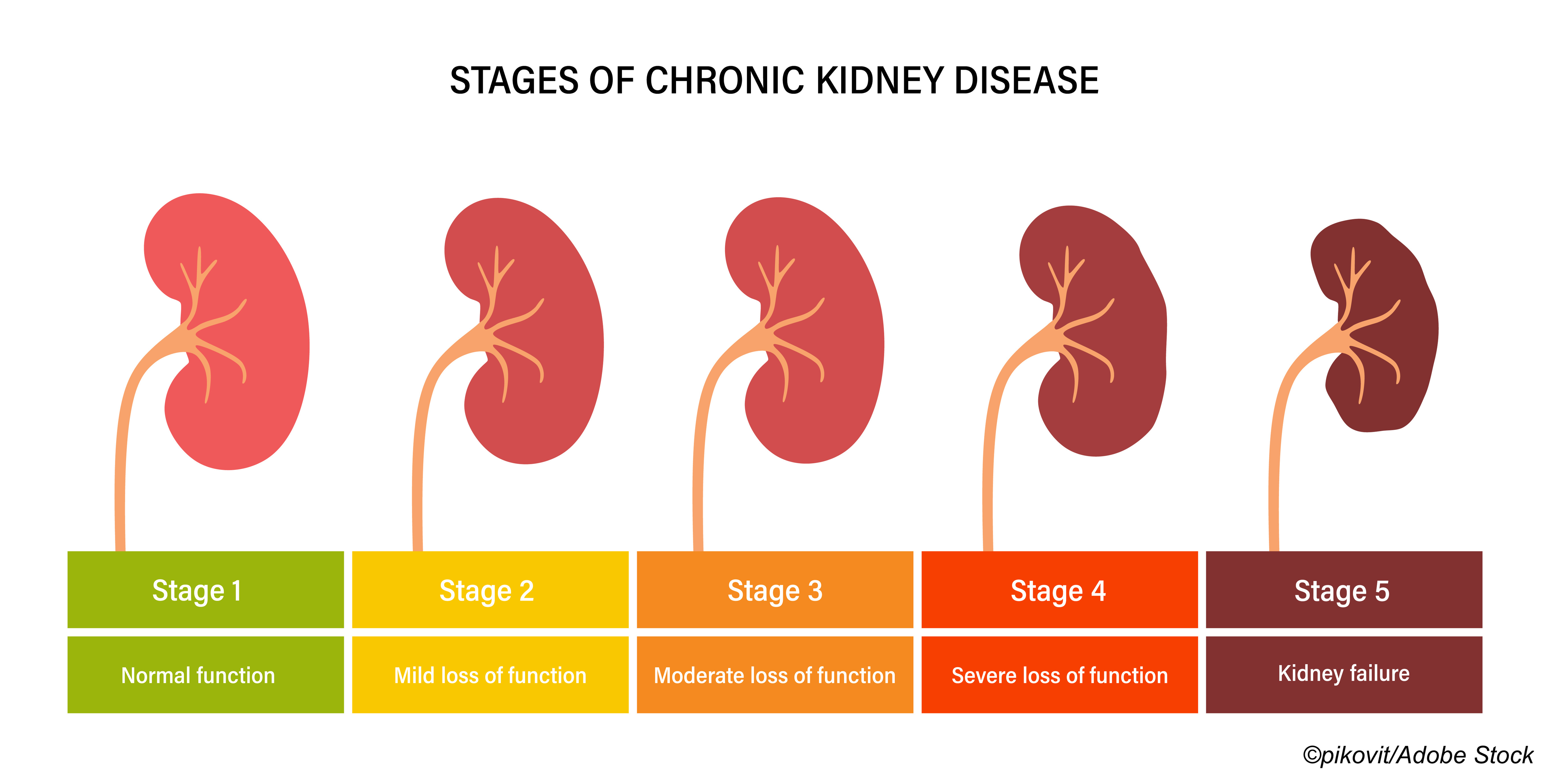
For the Chlorthalidone in Chronic Kidney Disease (CLICK) trial, Agarwal and fellow researchers randomized 160 patients with stage 4 chronic kidney disease and poorly controlled hypertension to chlorthalidone (initial dose: 12.5 mg/d, increased every four weeks as needed to a maximum dose of 50 mg/d) or placebo.
The primary outcome was change in 24-hour ambulatory systolic pressure from baseline to 12 weeks, and secondary outcomes included change in baseline urinary albumin-to-creatinine ratio, N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels, plasma renin levels, aldosterone levels, and total body volume.
Mean patient age was 66 years, 77%-78% were men, 76% had diabetes, and 60% were receiving loop diuretics. The primary causes of chronic kidney disease in most patients were diabetes (52% in chlorthalidone group, 53% in placebo group) and hypertension (32% and 33%, respectively). The baseline mean estimated glomerular filtration rates was 23.2 ml/min/1.73 m2, and mean number of antihypertensive medications was 3.4.
Agarwal and colleagues defined uncontrolled hypertension as a mean 24-hour ambulatory systolic BP ≥130 mmHg, or a diastolic BP ≥80 mmHg despite treatment with at least one antihypertensive medication.
Patients reported to clinics for nine prespecified trial visits. At randomization, mean 24-hour ambulatory systolic BP was 142.6 mmHg in patients randomized to chlorthalidone, and 140.1 mmHg in the placebo group. Mean 24-hour ambulatory diastolic BPs were 74.6 and 72.8 mmHg, respectively.
In patients treated with chlorthalidone, the adjusted change in 24-hour systolic BP from baseline to 12 weeks was −11.0 mmHg (95% CI: –13.9 to –8.1), compared with –0.5 mmHg (95% CI: –3.5 to 2.5) in placebo patients, for a between-group difference of –10.5 mmHg (95% CI: –14.6 to –6.4; P<0.001).
For the secondary outcome of urinary albumin-to-creatinine ratio from baseline, the percent change in patients treated with chlorthalidone was –41%, compared with –7% in the placebo group at 4 weeks (between-group difference: –36 percentage points; 95% CI: –49 to –21), and as follows at later time points:
- 8 weeks: –45% and –3%, respectively (between-group difference: –43 percentage points (95% CI: –54 to –28).
- 12 weeks: –52% and –4% (between-group difference: –50 percentage points; 95% CI: –60 to –37).
The following percent changes were seen in the NT-proBNP levels in patients treated with chlorthalidone versus placebo:
- 4 weeks: –25% versus –14%, respectively (between-group difference: –13 percentage points; 95% CI: –29 to 6).
- 8 weeks: –32% versus 5% (between-group difference: –35 percentage points; 95% CI: –48 to –20).
- 12 weeks: –30% versus –11% (between-group difference: –21 percentage points; 95% CI: –35 to –4).
Adverse events were seen in 91% of the chlorthalidone group compared with 86% of the placebo group. Treatment with chlorthalidone caused more frequent hypokalemia, reversible serum creatinine level increases, hyperglycemia, dizziness, and hyperuricemia. Researchers noted however, that these adverse events are known to be associated with chlorthalidone therapy.
“The change from baseline in the estimated GFR was –2.7 ml/min/1.73 m2 in the chlorthalidone group and 0 in the placebo group at 4 weeks after the initiation of the assigned regimen (between-group difference, –2.7 ml/min/1.73 m2, 95% CI, –3.9 to –1.6); –2.7 ml/min/1.73 m2 and 0.3 ml/min/1.73 m2, respectively, at 8 weeks (between-group difference, –3.0 ml/min/1.73 m22 and –0.5 ml/min/1.73 m2, respectively, at 12 weeks (between-group difference, –2.2 ml/min/1.73 m2
Agarwal also included an observational follow-up period of up to three years, which was initiated two weeks after treatment discontinuation. During this time, 20 patients treated with chlorthalidone and 29 patients treated with placebo experienced decreases in estimated GFR to ˂10 ml/min/1.73 m2, underwent long-term dialysis, or died (HR: 0.63; 95% CI: 0.36-1.12).
“Reductions in body weight, body volume, and plasma renin, aldosterone, and NT-proBNP levels within 4 weeks after starting chlorthalidone therapy suggest that the mechanism of blood-pressure reduction is consistent with the changes in body volume over time, which decreased during the treatment period and then increased after the regimen was discontinued. Two weeks after chlorthalidone therapy was discontinued, 44% of the reduction in seated clinic systolic blood pressure and 53% of the peak weight loss that was observed at the end of the 12-week treatment period remained,” concluded Agarwal et al.
They cautioned, however, that “Chlorthalidone should be used with caution in patients receiving loop diuretics, especially because of the risk of an increase in the serum creatinine level. The lowest dose of chlorthalidone produced most of the blood-pressure-lowering effect, and this might be the safest dose to use. A reduction in the dose of the loop diuretic might be needed.”
Study limitations include its small size and underrepresentation of women, Asian, and Hispanic patients.
-
In patients with advanced chronic kidney disease and poorly controlled hypertension, chlorthalidone therapy improved blood-pressure control at 12 weeks compared with placebo.
-
The percent change in the urinary albumin-to-creatinine ratio from baseline to 12 weeks was lower in the chlorthalidone group than in the placebo group by 50 percentage points.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This study was funded by the National Heart, Lung, and Blood Institute and the Indiana Institute of Medical Research.
Agarwal has served as a consultant for Akebia Therapeutics Inc., AstraZeneca AB, AstraZeneca Pharmaceuticals LP, Bayer HealthCare Pharmaceuticals Inc., Boehringer Ingelheim b.v., Boehringer Ingelheim Pharma GmbH & Co. KG, Boehringer Ingelheim Pharmaceuticals Inc., Eli Lilly and Company, Ironwood Pharmaceuticals Inc., Janssen Research & Development LLC, Lexicon Pharmaceuticals Inc., Merck, Reata, Relypsa Inc., Sanofi US Services Inc., Sanofi-Aventis U.S. LLC, and Vifor Fresenius Medical Care Renal Pharma Ltd. He also reported receiving travel considerations from Akebia Therapeutics, Bayer HealthCare Pharmaceuticals Inc., Boehringer Ingelheim Pharma GmbH & Co. KG, Boehringer Ingelheim Pharmaceuticals Inc., Merck, Reata, Relypsa Inc., Vifor Fresenius Medical Care Renal Pharma Ltd.; royalties from Wolters Klewer Health Inc.; and a gift from Otsuka America Pharmaceutical Inc.
Cat ID: 127
Topic ID: 81,127,730,6,914,127,541,192,925,540


Create Post
Twitter/X Preview
Logout