The American College of Cardiology and the American Heart Association have collaborated to issue a new guideline on coronary artery revascularization, and simultaneously published it in the Journal of the American College of Cardiology and Circulation.
This latest iteration—”2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization”—has been updated to incorporate six previous guidelines on coronary artery revascularization, as well as recent clinical data from trials of coronary artery revascularization. Guideline writers conducted a comprehensive literature search from May 2019 to September 2019 of PubMed, EMBASE, the Cochrane Collaboration, CINHL Complete, and other databases for relevant studies.
The new guideline replaces the 2011 coronary artery bypass graft surgery and the 2011 and 2015 percutaneous coronary intervention guidelines.
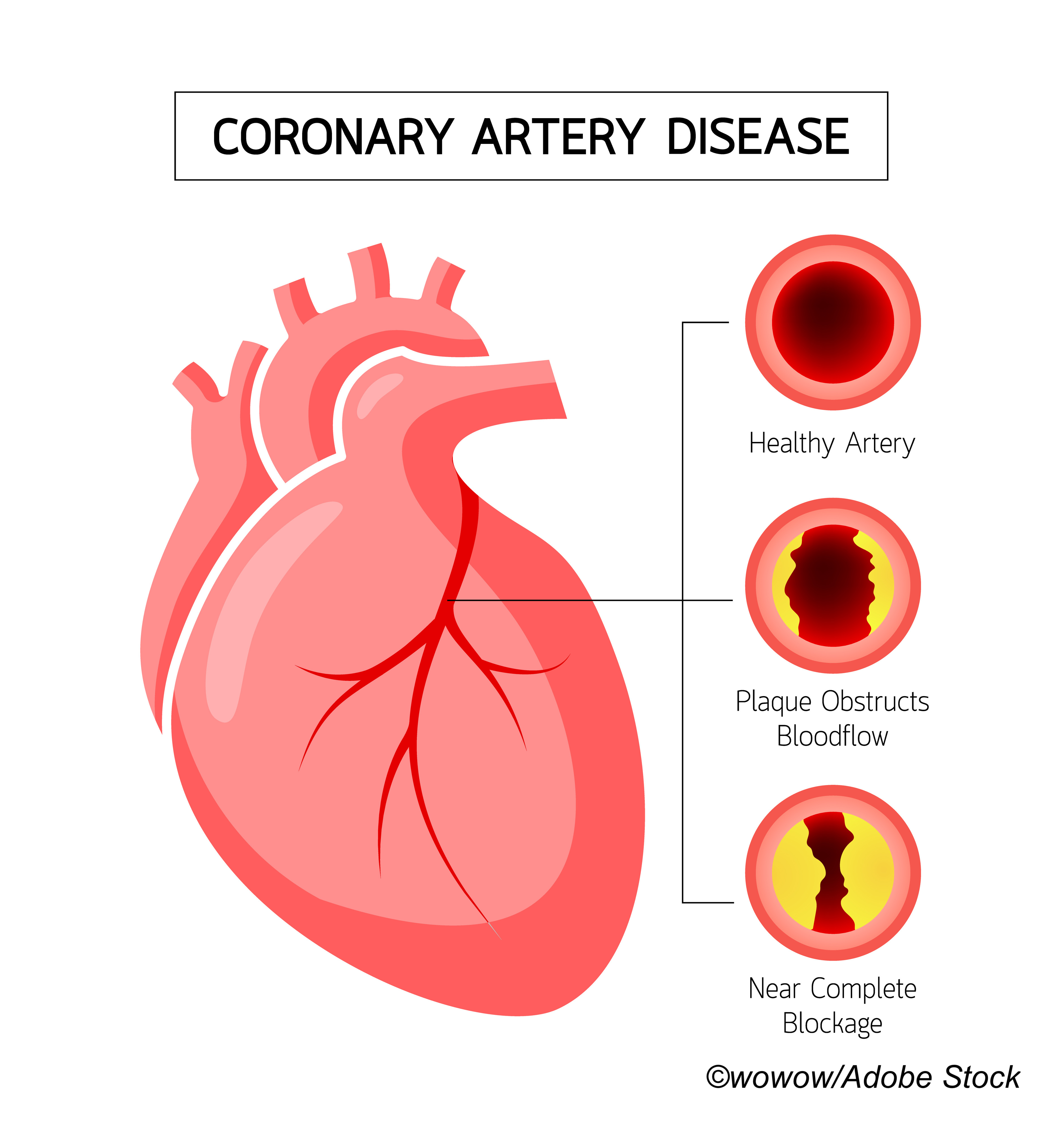
“Coronary artery disease [CAD] remains a leading cause of morbidity and mortality globally, and coronary revascularization is an important therapeutic option when managing patients with this disease,” said Jennifer S. Lawton, MD, guideline writing committee chair and professor of surgery and Chief of the Johns Hopkins Division of Cardiac Surgery, as well as Director of the Cardiac Surgery Research Laboratory. “Treatment recommendations in the guideline outline an evidence-based approach to managing patients with coronary artery disease who are being considered for coronary revascularization, with the intent to improve quality of care and align with patients’ interests.”
Reducing disparities in care was a particular focus in this guideline, which emphasizes that the use of invasive heart procedures such as coronary artery revascularization should not be limited in women and adults from varying racial and ethnic groups, as studies have shown that patients experience similar outcomes regardless of gender or race.
Lawton and fellow guideline writers also emphasized the need to base revascularization treatment decisions for CAD on clinical indications and stressed the importance of establishing a multidisciplinary Heart Team that also incorporates the patient and the patient’s preferences. This team should include a cardiologist, cardiac surgeon, other specialists, and the patient.
“The Heart Team has become an important paradigm in clinical practice, emphasizing the importance of team consensus on the optimal approach to revascularization,” said Jacqueline E. Tamis-Holland, MD, guideline writing committee vice-chair and professor of medicine at the Icahn School of Medicine at Mount Sinai.
Top recommendations in the new guideline include the following:
- Base treatment decisions on coronary revascularization in patients with CAD on clinical indications regardless of sex, race, or ethnicity to reduce disparities of care.
- When the optimal treatment strategy is not clear, employ a multidiscliplinary Heart Team approach to make treatment decisions that are patient centered and include shared decision-making.
- Surgical revascularization is indicated in patients with significant left main disease over medical therapy. In those with low to medium anatomic CAD complexity, percutaneous revascularization is a viable option.
- In patients with stable ischemic heart disease, normal left ventricular ejection fraction, and triple-vessel CAD, updated data from recent studies add to older data that support the mortality benefits of revascularization. Base decisions for revascularization on disease complexity, technical feasibility, and discussions with a Heart Team.
- Choose a radial artery as a surgical revascularization conduit over a saphenous vein conduit to bypass the second most important target vessel showing significant stenosis after the left anterior descending coronary artery for superior patency, improved survival, and fewer adverse cardiac events.
- Use radial artery access in patients with acute coronary syndrome or stable ischemic heart disease undergoing percutaneous intervention to reduce bleeding and vascular complications.
- Prescribe a short duration of dual antiplatelet therapy after percutaneous revascularization in patients with stable ischemic heart disease to reduce the risk of bleeding. After 1-3 months of dual antiplatelet therapy, some patients can transition to P2Y12 inhibitor monotherapy and discontinue aspirin.
- Improve outcomes in patients with significantly stenosed nonculprit artery and ST-segment-elevation myocardial infarction with staged percutaneous intervention, in hospital or after discharge.
- Use a Heart Team approach to make revascularization decisions in patients with diabetes and multivessel CAD. In these patients with triple-vessel disease, surgical revascularization is recommended, and in those who are poor surgical candidates, percutaneous coronary intervention can be considered.
- Calculate surgical risks in patients undergoing surgical revascularization of CAD using the Society of Thoracic Surgeons score.
According to the ACC/AHA, this new revascularization guideline complements the recently released 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain, because revascularization is often a treatment option for patients with chest pain.
“This is part of a strategic effort by the ACC and AHA to approach guidelines from a real-practice perspective, rather than solely topic-based guidelines,” according to the ACC/AHA.
-
New ACC/AHA guideline on coronary revascularization updates and incorporates six previous guidelines in outlining preferred approaches and treatments for patients with CAD needing coronary artery revascularization.
-
Equitable treatment of women and people from diverse racial or ethnic groups and the formation of a Heart Team receive particular emphasis.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
Writing committee members are required to recuse themselves from voting on sections to which their specific relationships with industry may apply.
Cat ID: 103
Topic ID: 74,103,730,103,232,308,914,192,925