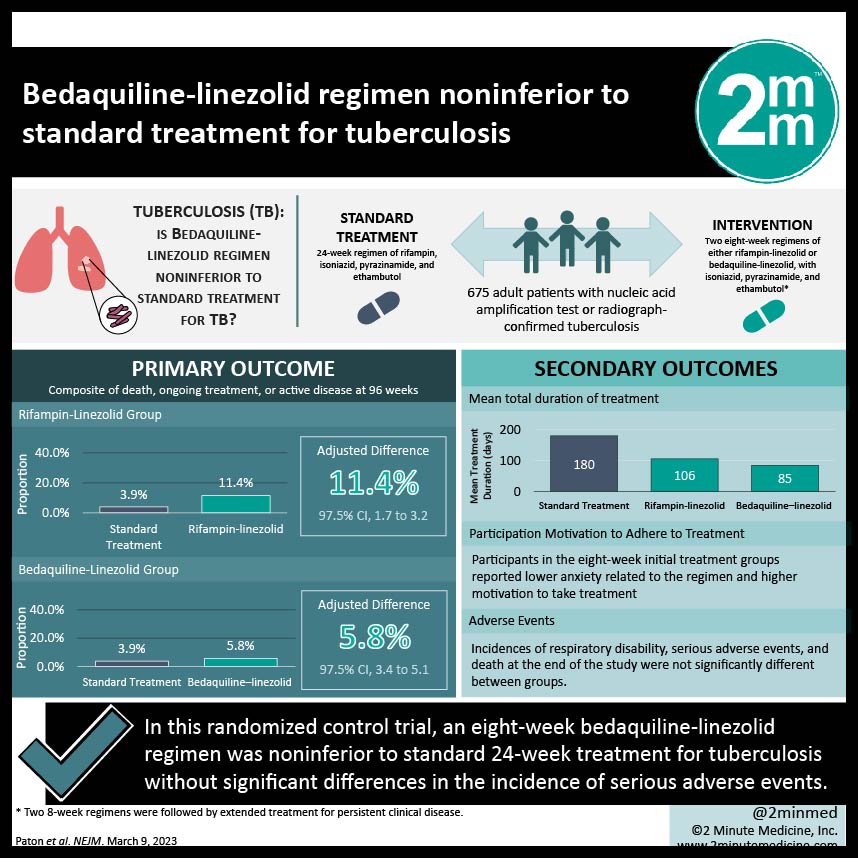
1. In this randomized control trial, an eight-week bedaquiline-linezolid regimen was noninferior to standard 24-week treatment for tuberculosis.
2. The incidence of serious adverse events was not significantly different between the bedaquiline-linezolid regimen and standard treatment.
Evidence Rating Level: 1 (Excellent)
Study Rundown: The current standard of treatment for tuberculosis is a six-month rifampin-based regimen. While it is effective in clinical trials, difficulty with long-term treatment adherence has led to reduced efficacy in real-world program implementation. In addition, at least 85% of clinical trial participants are cured within three to four months of treatment. The entire six-month regimen may lead to overtreatment in most patients. In this noninferiority open-label randomized control trial, initial therapy with two eight-week regimens followed by extended treatment for persistent clinical disease, monitoring after treatment, or retreatment for relapse was compared with a standard 24-week regimen for adult patients with tuberculosis. The two eight-week regimens were rifampin-linezolid or bedaquiline-linezolid combined with isoniazid, pyrazinamide, and ethambutol. Patients were followed for 96 weeks. For the primary outcome, a composite of death or ongoing tuberculosis treatment or active tuberculosis by week 96, the noninferiority criterion was met for the group with an initial bedquiline-linezolid regimen and not for the group with an initial rifampin-linezolid regimen. The shorter duration regimens also had a positive effect on participant motivation to adhere to treatment. As a limitation, this was an open-label design, which may introduce treatment bias.
Click to read the study in NEJM
Relevant Reading: Four-Month Moxifloxacin-Based Regimens for Drug-Sensitive Tuberculosis
In-Depth [randomized controlled trial]: In this noninferiority, open-label, randomized controlled trial, adult patients (n = 675) with nucleic acid amplification test or radiograph-confirmed tuberculosis were randomized to receive one of four eight-week initial treatment regimens [rifampin-linezolid (n=184); bedaquiline-linezolid (n=189); rifapentine-linezolid (n=78); rifampin-clofazimine (n = 42)] or standard treatment (n=181). The rifapentine-linezolid and rifampin-clofazimine groups did not achieve complete enrollment. For the eight-week initial regimens, treatment was continued for persistent or relapse of clinical disease. Patients were followed for 96 weeks. For the primary outcome, a composite of death, ongoing treatment, or active disease at 96 weeks, the noninferiority criterion compared to the standard treatment (3.9%) was not met in the rifampin-linezolid group (11.4% adjusted difference; 7.4 percentage points; 97.5% Confidence Interval [CI], 1.7 to 3.2) and met in the bedquiline-linezolid group (5.8% adjusted difference; 0.8 percentage points; 97.5% CI -3.4 to 5.1). For the patient-centered secondary outcomes, the mean total duration of treatment was 180, 106, and 85 days for the standard, rifampin-linezolid, and bedaquiline-linezolid groups, respectively. Participants in the eight-week initial treatment groups reported lower anxiety related to the regimen and higher motivation to take treatment. Incidences of respiratory disability, serious adverse events, and death at the end of the study were not significantly different between groups. This study suggests that there may be value in shifting the tuberculosis management strategy from a 24-week regimen to a shorter regimen.
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.