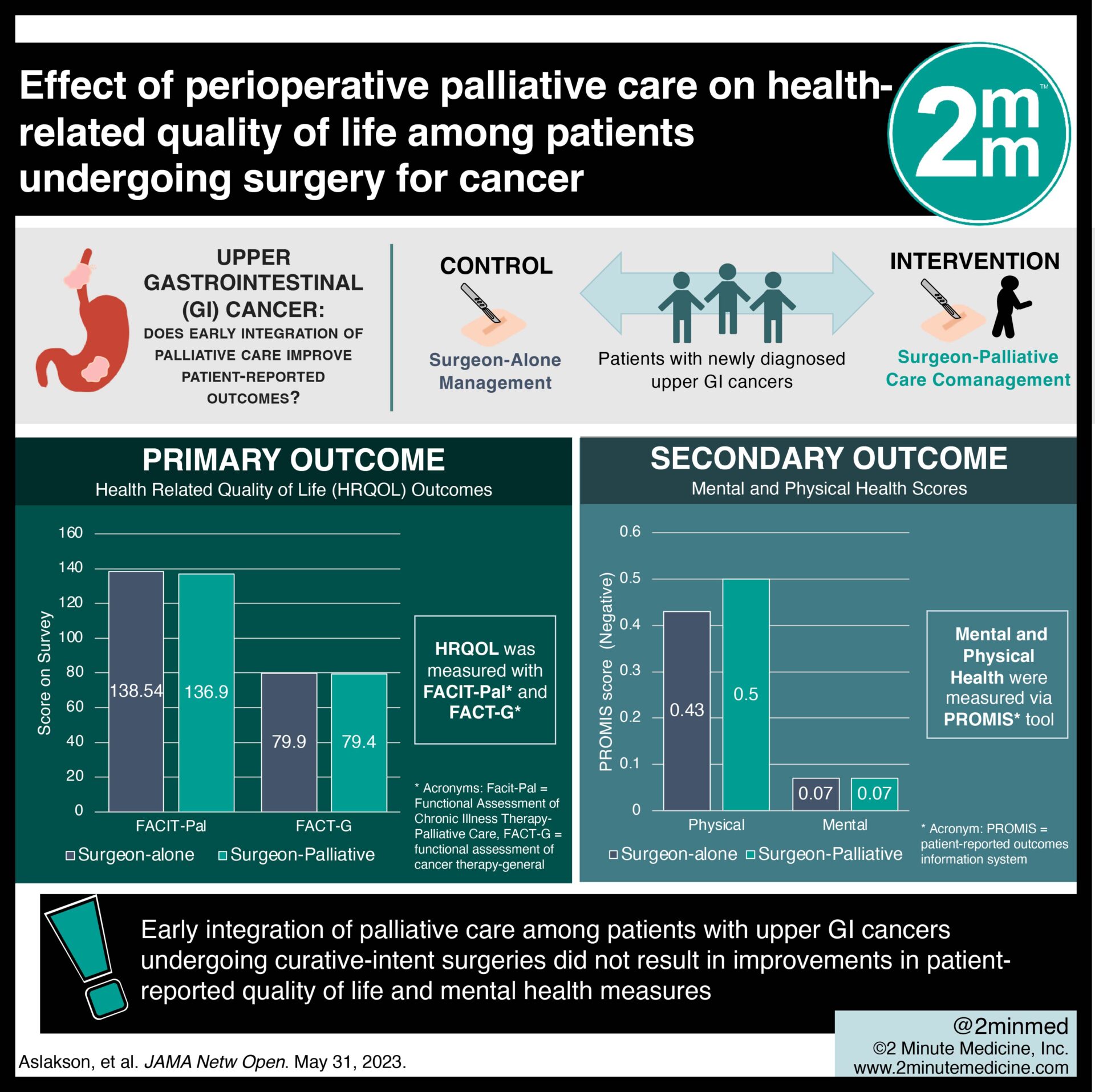
1. In this randomized controlled trial, early integration of palliative care among patients with upper gastrointestinal (GI) cancers undergoing curative-intent surgeries did not result in improvements in patient-reported quality of life and mental health measures
Evidence Rating Level: 1 (Excellent)
Study Rundown: GI cancers often require extensive surgeries and can lead to significant morbidity and mortality. Palliative care entails symptom management and psychosocial support to individuals with serious illness to optimize their quality of life, regardless of diagnosis, prognosis, or care goals. While medical oncology studies have demonstrated the benefits of palliative care on diverse patient-report outcomes, there is a paucity of literature surrounding proactive palliative care in surgical oncology patients. This randomized clinical trial aimed to assess the effect of integrating palliative care with standard surgical oncology care on patient-reported outcomes. From October 2018 to March 2022 patients across five medical centers with newly diagnosed upper GI cancers were enrolled and randomly assigned to receive either surgeon-alone management (standard care) or surgeon-palliative care comanagement (intervention). Patient questionnaires were utilized to assess health-related quality of life (HRQOL) outcomes. There was no significant difference in HRQOL outcomes at 3 months postoperative between the study groups. Overall, this clinical trial does not support that the early integration of palliative care among patients with upper GI cancers undergoing curative-intent surgeries lead to improvement in patient-reported outcomes.
In-depth [randomized-controlled trial]: Patients with upper GI cancers undergoing extensive curative-intent surgical resections often necessitate postoperative admission to the ICU and patients may experience persistent pain, decreased quality of life, compromised global health, impaired emotional and social functioning, decreased appetite and high rates of cancer-related mortality. Multiple studies demonstrate that palliative care improves patient-reported outcomes among the medical oncology patient population, however its impact in a surgical oncologic patient population has not been evaluated. From October 2018 to March 2022, patients with newly diagnosed upper GI cancers who were scheduled for curative-intent surgery across five medical centers in the United States were invited to participate in the study. A total of 359 patients (mean [SD] age, 64.7 [10.4] years; 90 women [51.4%] and 85 men [51.4%]) were randomized in a 1:1 ratio to receive surgeon-alone management or the study intervention — surgeon-palliative care comanagement. Patients assigned to the intervention group had scheduled meetings with a specialist from the palliative care team before surgery and at various intervals after surgery (1 week, 1 month, 2 months, and 3 months), with additional visits organized at the discretion of the patient, surgery team or palliative care team. HRQOL was measured with the Functional Assessment of Chronic Illness Therapy-Palliative Care (FACIT-Pal) Subscale and Functional Assessment of Cancer Therapy–General (FACT-G) , which has been used extensively as a quality-of-life measure in previous medical oncology studies. Mental and physical health scores were calculated from the 29-item Patient-Reported Outcomes Measurement Information System (PROMIS) tool. Among 182 patients randomized to the intervention, 90% received at least 1 palliative care visit with a mean (SD) of 3.43 (1.70) of the 5 total possible visits during the first 3 months postoperative. Among 177 patients randomized to the control group, 11.3% had a palliative care consultation during the first 3 months. When comparing HRQOL at 3 months following the operation, there were no significant differences between the study groups (FACIT-Pal, 138.54 [28.28] vs 136.90 [28.96]; P = .62; FACT-G, 79.90 [17.14] vs 79.40 [17.45]; P = .80; PROMIS-29 physical health, −0.43 [0.89] vs −0.50 [1.01]; P = .56; PROMIS-29 mental health, −0.07 [0.87] vs −0.07 [0.84]; P = .98). There was also no significant difference in 3-month mortality between the groups (P > .99). Overall, these findings suggest that early integration of palliative care does not improve patient-reported HRQOL or mood symptoms. These results may have been limited by the overwhelming preference of telephone-based palliative care in the intervention group, particularly after March 2020 when all outpatient palliative care was conducted via telephone due to the COVID-19 pandemic. Delivery of palliative care through telephone consultations, may have resulted in a lower “dose” of care and thereby smaller impact on the measured outcomes.
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.