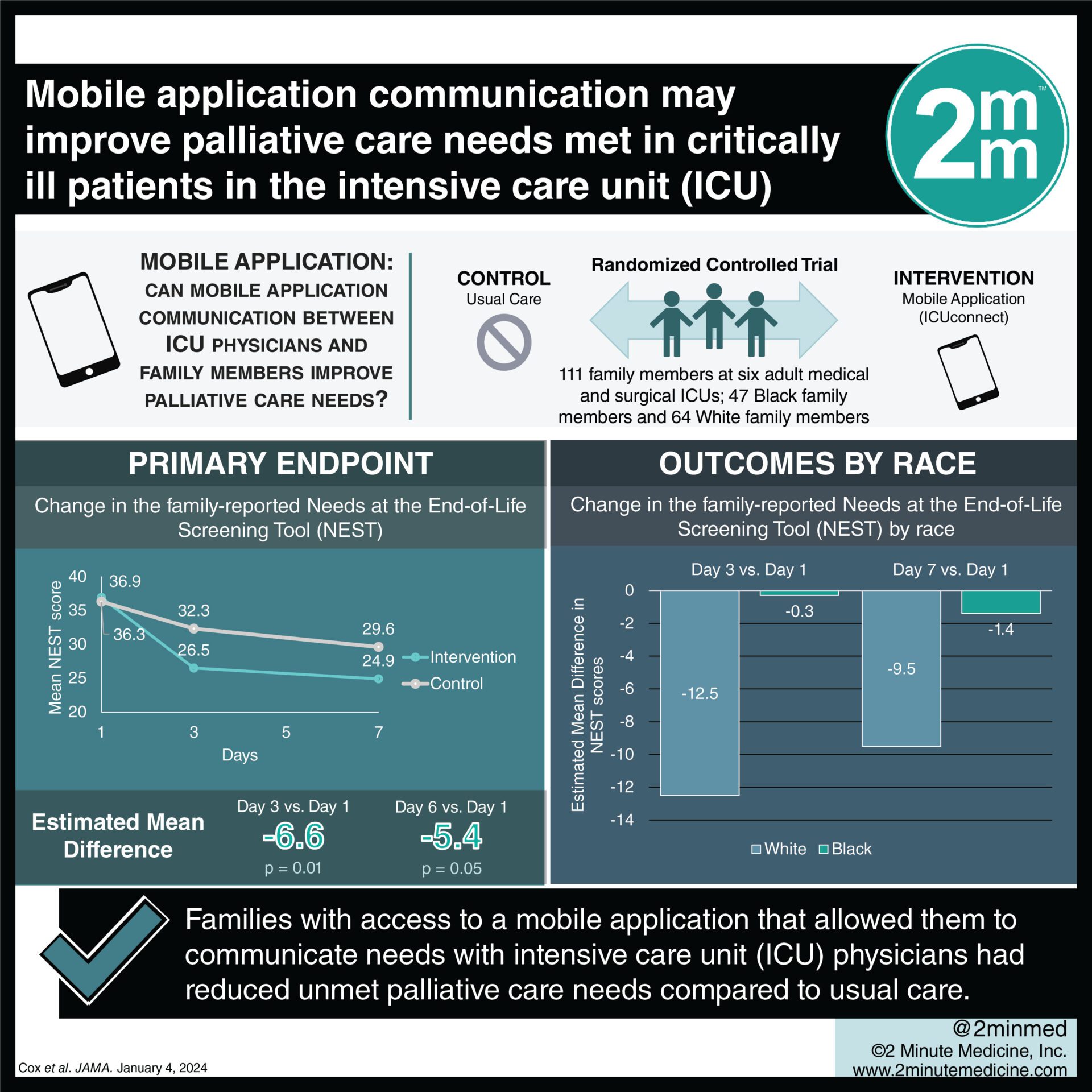
Families with access to a mobile application that allowed them to communicate needs with ICU physicians had reduced unmet palliative care needs.
1. Families randomized to having access to a mobile application that allowed them to communicate needs with intensive care unit (ICU) physicians were found to have reduced unmet palliative care needs compared to usual care.
2. White families were observed to benefit more from the intervention than Black families as measured by the Needs at the End-of-Life Screening Tool (NEST) score.
Evidence Level Rating: 1 (Excellent)
There is a desperate need for more palliative care specialists globally as evidenced by the burden ICU patients experience. This burden is disproportionately harming black patients and their families, showing the unmet palliative care needs. In this randomized controlled trial involving 6 adult medical and surgical ICUs in North Carolina, patient-family dyads were randomly assigned access to a mobile application (ICUConnect) that allowed them to communicate palliative care needs directly to ICU attending physicians. The study focused on the change in the family-reported Needs at the End-of-Life Screening Tool (NEST) score. 111 family members and 111 patients were enrolled in the study under the supervision of 37 physicians. The primary outcome revealed a noteworthy reduction in NEST scores among intervention recipients at both day 3 (estimated mean difference -6.6 points, P = 0.01) and day 7 (estimated mean difference -5.4 points, P = 0.05) compared to the control group. Interestingly, white families benefited more from the intervention than Black families as can be seen by their improved NEST scores at days 3 (estimated mean difference -12.5 points vs -0.3 points) and 7 (estimated mean difference -9.5 points vs -1.4 points). Study findings suggest that the use of a mobile communication application may have use-cases in the improvement of palliative care outcomes in the ICU. Additionally however, they also provide further insights into the potential roles that implicit biases and race may play in the quality of care provided to palliative care patients and their families.
Click to read the study in JAMA Network Open
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc