The analysis found that the annualized relapse rate was 0.09 among the patients on ofatumumab compared with a rate of 0.18 among the users of teriflunomide — which translated to a 50.3% relative risk reduction (P<0.001), said Stephen Hauser, MD, the Robert A. Fishman Distinguished Professor of Neurology and director of the Weill Institute for Neurosciences at University of California at San Francisco.
“Ofatumumab is the first FDA-approved high efficacy disease-modifying therapy that can be self-administered at home, as demonstrated in the phase III ASCLEPIOS trials,” Dr. Hauser says in his presentation at the 2020 virtual joint meeting of the American Committee for Treatment and Research in Multiple Sclerosis (ACRTRIMS) and the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
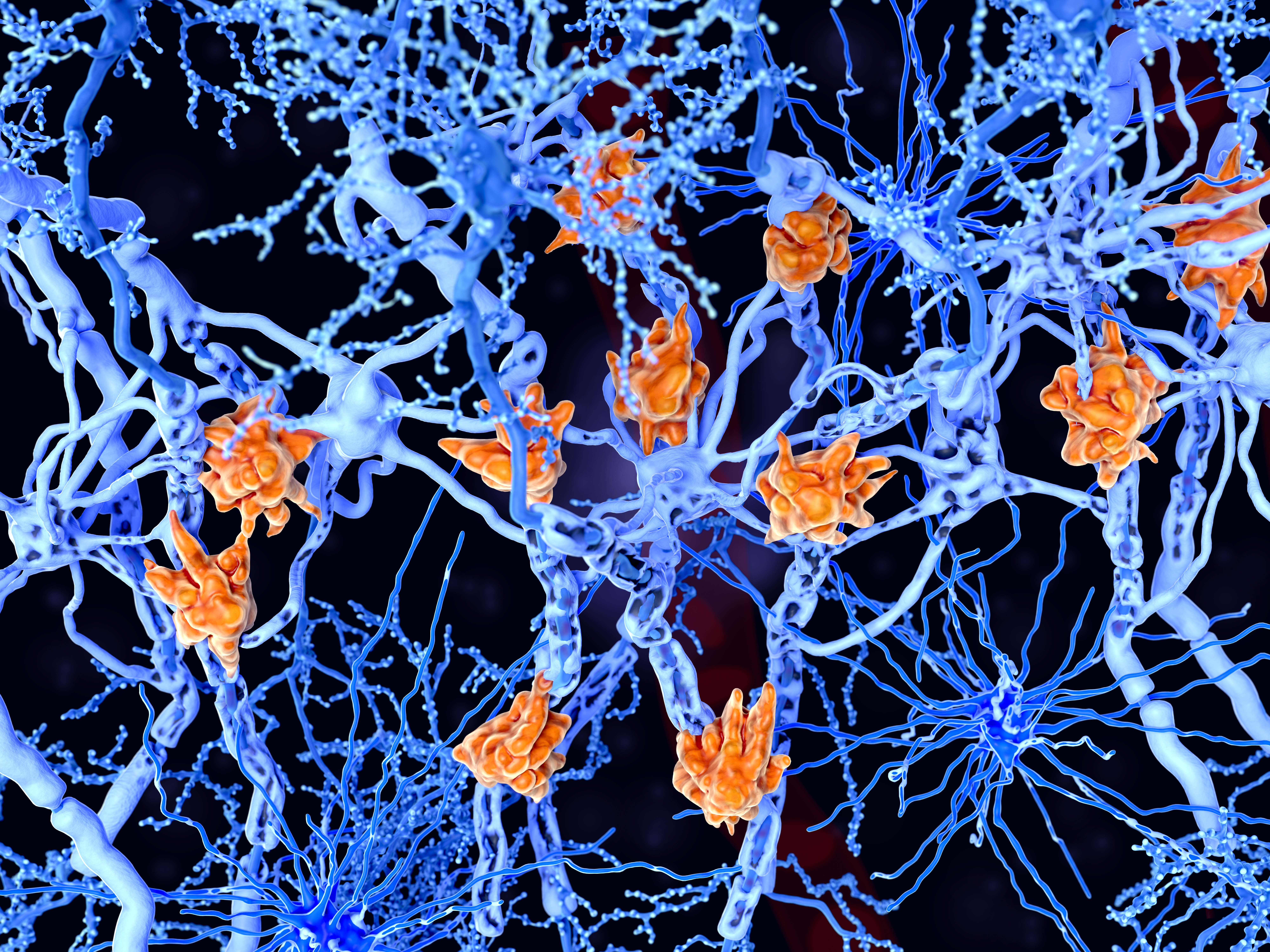
“Despite the availability of many disease-modifying therapies for treatment of relapsing multiple sclerosis, there remains an unmet need for highly efficacious therapies that have a favorable safety profile and are easy to use,” he says.
In addition to reducing the relapse rate, Dr. Hauser said the risk of confirmed disability worsening at 3 months was reduced 38% with ofatumumab compared with teriflunomide (P=0.065), and the risk of confirmed disability worsening at 6 months was reduced 46% (P=0.044).
The researchers also reported that, in the subgroup analysis, treatment with ofatumumab was associated with significant reductions in gadolinium-positive T1 scans — a reduction of 95% (P<0.001); in the T2 lesions seen per year — a reduction of 82% (P<0.001); and in the T2 lesions seen at two years — a reduction of 97% (P<0.001).
Dr. Hauser said there were no imbalances between the two groups in serious adverse events, although there were 2 serious infections among the teriflunomide patients and 6 serious infections among the ofatumumab patients.
“No opportunistic infections such as progressive multifocal leukoencephalopathy (PML) and hepatitis B reactivation were observed,” Dr. Hauser reports.
In the naïve-treatment population, 98.8% of patients were compliant with the treatment regimen, similar to the 98.3% of patients being compliant with the regimen in the overall trial.
In the ASCLEPIOS trials, ofatumumab was administered subcutaneously on day 1 of treatment, and then on day 7 and day 14, after which patients received doses every 4 weeks. Treatment with ofatumumab was compared with patients taking oral teriflunomide daily. The patients were evenly matched, with an average age of 36 years; about 67% of the patients were women. Their average Expanded Disability Status Scale score was 2.3, and at baseline, the patients had been averaging 1.4 relapses per year.
In the subgroup analysis, researchers identified patients in the phase III ASCLEPIOS I/II trials who were diagnosed with early relapsing multiple sclerosis. Of the 1,882 patients in the parent studies, the subgroup analysis scrutinized outcomes in 615 patients — about 32.7% of the total, Dr. Hauser says.
In commenting on the study, Asaff Harel, MD, assistant professor of neurology at Lenox Hill Hospital/Hofstra School of Medicine/Northwell Health, New York City, says, “This is a subgroup analysis of the newly FDA-approved B-Cell therapy that is administered subcutaneously once a month. The idea is that it allows people to take control of their own schedule if they want.”
Dr. Harel said the injections are similar to people with diabetes taking insulin injections, and self-injection is common among older multiple sclerosis patients who have been on injectable medications for that disease.
“The good news about this is that the treatment is just once monthly, and the injection site reactions reported in the study were much milder than what we have observed with other medications,” he says. “They found, on the whole, that annualized relapse rates were reduced in the entire study, so they wanted to look at this sub-group analysis, looking specifically at young individuals that have early relapsing-remitting multiple sclerosis.”
Dr. Harel noted that this particular group of patients did not have experience with subcutaneous injections, so that made it an interesting group to analyze. “Compliance appeared to be really, really good, and I think that speaks to the fact that the injection site reactions weren’t too bad.”
“We know that ofatumumab is a highly-efficacious option, and this analysis shows us that even as a first-line option and with relatively small numbers, there was still an effect in slowing disability compared to teriflunomide,” he says.
- In relatively young multiple sclerosis patients who were treatment naïve, compliance with ofatumumab was very high.
- As a subgroup analysis, the findings from this study should be viewed with caution until it is published in a peer-reviewed journal.
Edward Susman, Contributing Writer, BreakingMED™
The study was sponsored by Novartis Pharma AG, Basel, Switzerland.
Hauser disclosed relationships with Anexxon, Alector, Bionure, Neurona, F. Hoffman-LaRoche, and Novartis.
Harel disclosed relationships with Biogen, Banner Life Sciences, and Alexion.
Cat ID: 708
Topic ID: 98,708,728,791,730,36,709,192,481,708



Create Post
Twitter/X Preview
Logout