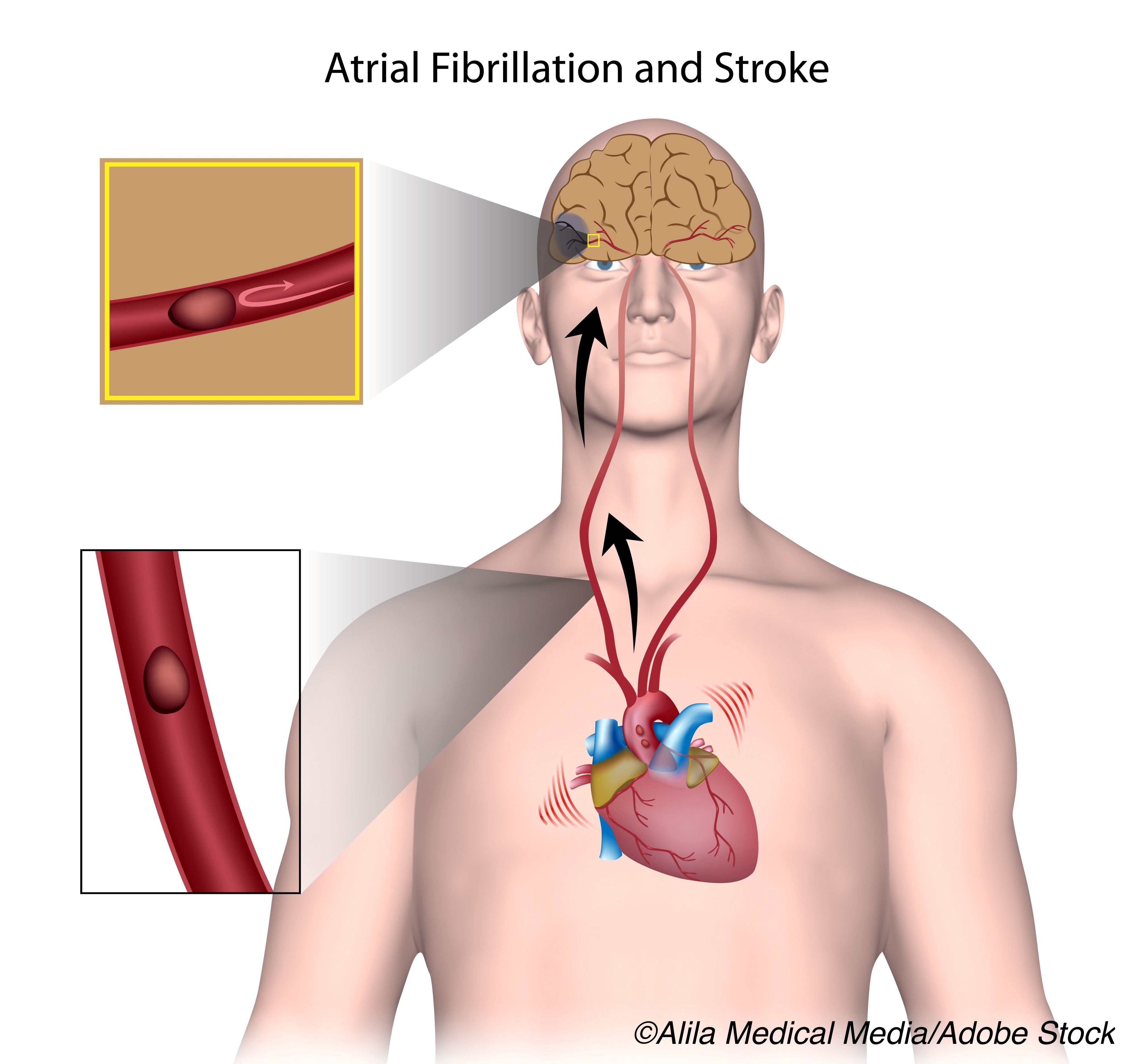
People with atrial fibrillation (AFib) detected after ischemic stroke (AFDAS) had higher mortality risk than people who had known atrial fibrillation (KAF) or no AFib at the time of ischemic stroke, a prospective study found.
“The AFDAS group had the highest risk of death, which was not explained by comorbidities or use of antithrombotic therapies,” wrote Rajat Deo, MD, MTR, of the University of Pennsylvania in Philadelphia, and co-authors in Neurology.
The researchers classified 1,489 patients with incident first ischemic stroke into four groups: no AFib (n=985), KAF (AFib known before the index stroke, n=215), AFDAS diagnosed within 6 months post-stroke (AFDAS ≤ 6 months, n=160), and AFDAS identified beyond 6 months post-stroke (AFDAS> 6 months, n=129).
Over median 4.9-year followup, there were 686 deaths. Regression models adjusted for use of antithrombotic agents showed:
- The AFDAS ≤ 6 months group had the highest independent risk of all-cause mortality after multivariable adjustment (HR 1.62, 95% CI 1.22-2.14).
- Patients in the no AFib group had similar mortality risk to KAF after adjustment.
- Both AFDAS ≤ 6 months (HR 1.62, 95% CI 1.22- 2.14) and AFDAS > 6 months (HR 1.42, 95% CI 1.07-1.88) were associated with increased risk of death relative to no AFib.
- For the combined AFDAS groups, a > 50% increased risk of death compared to the no AFib group was seen after controlling for demographics, clinical risk factors, anticoagulation, and antiplatelet therapies.
“Our data suggest that 40-60% of post-stroke patients, who eventually have a diagnosis of AFib, are treated with anticoagulation,” the investigators wrote.
The study “highlights that AFib is often diagnosed late after the index stroke; these patients are at increased risk of death; and a significant proportion of them do not take anticoagulants despite their known efficacy and safety for stroke prevention,” noted Luciano Sposato, MD, MBA, of Western University in London, Canada, and David Seiffge, MD, of the University Hospital Inselspital, in Bern, Switzerland, in an accompanying editorial.
“These findings suggest that post-stroke care needs innovation and improvement,” Sposato and Seiffge added. “Prospectively refining our understanding of AFDAS in different cohorts is needed to more accurately estimate the magnitude and the direction of its association with clinical outcomes.”
About 80% of people who had ischemic stroke do not have known AFib, and of these about a quarter are found to have newly diagnosed AFib after appropriate electrocardiographic monitoring, making AFDAS important as a distinct clinical entity.
While neurogenic AFDAS is a lower-risk arrhythmia due to inflammation and impairment of autonomic networks, cardiogenic AFDAS is an undetected arrhythmia detected after stroke that carries higher risk.
Although the prevalence of cardiovascular comorbidities that increase stroke risk is lower in AFDAS than KAF, inconsistent findings have emerged from prior research regarding whether stroke recurrence with AFDAS differs from those without AFib or not.
In the present study, Deo and colleagues prospectively followed adults who had electrocardiograms (ECG) between June 2004 and December 2009 at their institution for incident stroke. They determined death through the National Death Index until June 2017.
Use of anticoagulants and antiplatelets were tracked during the study, including warfarin and non-vitamin K antagonists (dabigatran, rivaroxaban, and apixaban) and aspirin, clopidogrel, or dipyridamole. Mean age and percent males were 63 years and 43% men for no AFib, 67 years and 51% men for KAF, 67 years and 59% men for AFDAS ≤ 6 months, and 67 years and 60% men for AFDAS > 6 months.
Annualized mortality rate was 8.8% in the no AFib group, 12.2% in the KAF group, 15.8% in the AFDAS ≤ 6 months, and 12.7% in the AFDAS > 6 months.
The no AFib group was more likely to have the lowest prevalence of heart failure, coronary heart disease, and chronic kidney disease. Those with KAF had the highest burden of comorbidities. In the overall AFDAS group, those with AFDAS ≤ 6 months were more likely to have heart failure, coronary heart disease and less likely to have diabetes or hypertension than those with AFDAS > 6 months.
In the KAF group, 29% were using anticoagulation prior to incident stroke and an additional 30% were started on anticoagulation after stroke. The use of oral anticoagulants and antiplatelet agents among those with AFDAS ≤ 6 months were 43% and 64%, respectively; for AFDAS > 6 months, 57% and 85%, respectively.
Anticoagulation use was documented in 15% to 23% of patients with AFDAS before AFib was first diagnosed in the study.
“The increased risk of death associated with AFDAS relative to no AFib in [the study] does not contradict previous investigations showing a low adjusted risk of stroke recurrence,” the editorialists observed, noting that stroke recurrences and post-stroke deaths are caused by different mechanisms.
About half of deaths in AFib patients are related to non-vascular causes, while only 16% of all-cause mortality is stroke-related, they pointed out, adding that the population in the present study had a high rate of cardiovascular comorbidities and misclassification may have resulted in added risk of death.
“It is possible that some KAF cases were not ascertained before stroke occurrence and were eventually misclassified as AFDAS,” they added, noting that 15% to 23% of patients with AFDAS were already receiving oral anticoagulants before AFDAS detection, suggesting some people may have had KAF that was missed.
Limitations of the study include a lack of systematic ECG monitoring. The researchers also did not adjust for the severity or topography of the initial stroke in their analysis.
-
People with atrial fibrillation (AFib) detected after ischemic stroke had higher mortality risk than people who had known atrial fibrillation or no AFib at the time of ischemic stroke, a prospective study found.
-
Patients with AFib discovered ≤ 6 months after the index stroke had the highest independent risk of all-cause mortality, after adjusting for demographics, clinical risk factors, and use of antithrombotic therapies.
Paul Smyth, MD, Contributing Writer, BreakingMED™
Partial support for this study was provided by the Winkelman Family Fund in Cardiovascular Innovation.
Deo reported no disclosures.
Sposato reported speaker and consulting honoraria from Boehringer Ingelheim, Pfizer, Bayer and Gore, research grants from Boehringer Ingelheim and Bayer, chair of the Brain & Heart Task Force of the World Stroke Organization, member of the editorial board of Neurology and Stroke journals, and member of the leadership group of the World Stroke Academy.
Seiffge reported being on advisory boards for Bayer and Portola/Alexion.
Cat ID: 2
Topic ID: 74,2,730,2,745,8,130,38,748,192,925



Create Post
Twitter/X Preview
Logout