Ramped-up lab surveillance and fast-track investigations helped put the brakes on the transmission of Candida auris (C. auris) in high-risk facilities in one California county, researchers reported.
In a study done at ventilator-capable skilled-nursing facilities (vSNFs) and long-term acute care hospitals (LTACHs) in Orange County, initial point prevalence surveys (PPS) identified 44 additional patients with C. auris in 100% of the LTACHs and 43% of the vSNFs, with the first bloodstream infection reported in May 2019, according to Ellora Karmarkar, MD, of the California Department of Public Health, CDC, in Richmond, and co-authors.
“By October 2019, a total of 182 patients with C. auris were identified by serial PPS and discharge testing. Of 81 isolates that were sequenced, all were clade III and highly related,” they wrote in the Annals of Internal Medicine.
The authors also found that assessments of infection-and-prevention control practices (IPC) showed “gaps in hand hygiene, transmission-based precautions, and environmental cleaning.” Nonetheless, the “outbreak was contained to 2 facilities by October 2019.”
The investigation improved IPC practices across facilities and likely mitigated transmission of C. auris within and outside [Orange County],” they concluded. “Public health oversight of interfacility communication during patient transfers also enabled proactive attention to IPC practices at receiving facilities and limited the risk for transmission.”
Karmarkar’s group pointed out that U.S. LTACHs and vSNFs have historically been susceptible to outbreaks of C. auris, and transmission was certainly exacerbated by the pandemic in the entire state.
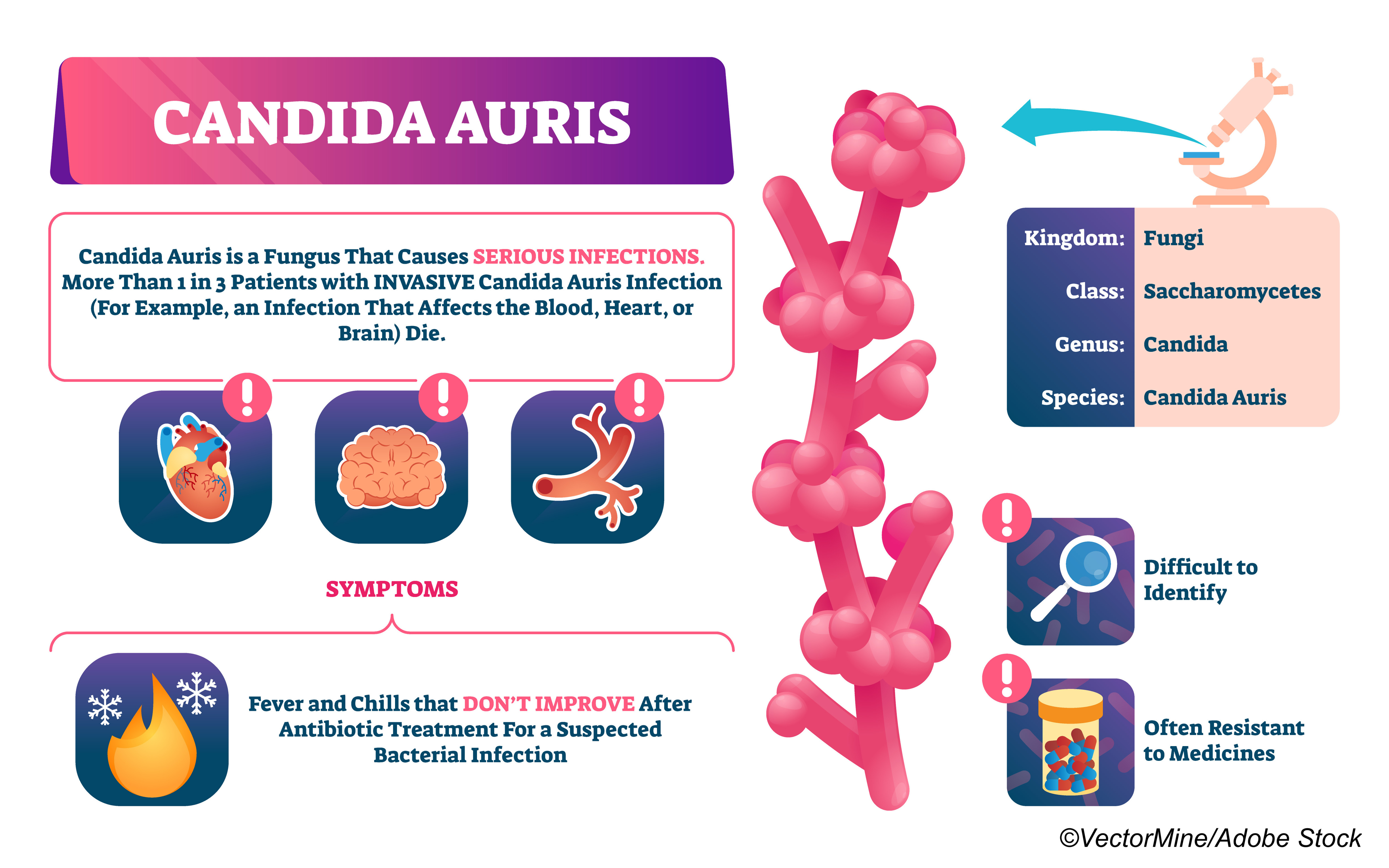
In an editorial accompanying the study, Lona Mody, MD, of the University of Michigan Medical School, and Marco Cassone, MD, PhD, of Michigan Medicine, both in Ann Arbor, noted that in “high-risk populations, such as Covid-19 patients requiring mechanical ventilation, C. auris may have surpassed C. albicans as a cause of candidemia, a disease with high lethality burden.”
Confirmed cases of Covid-19-related C. auris were seen in Brazil in late 2020, and described in a brief report in the Journal of Fungi, with the reporting authors explaining that the “travel restrictions during the Covid-19 pandemic and the absence of travel history among the colonized patients lead to the hypothesis that this species was introduced several months before the recognition of the first case and/or emerged locally in the coastline Salvador area [of Brazil].”
Risk factors for candidemia in Covid-19 patients include long hospital stays, invasive and surgical procedures (urinary and central venous catheters), and broad-spectrum antibiotics and corticosteroids.
“The virus can damage the intestinal mucosa of severe Covid-19 patients [facilitating invasion of the bloodstream by pathogens] so that the patient becomes vulnerable to candidemia,” explained Arnaldo Colombo, MD, PhD, of the Federal University of São Paulo (UNIFESP), in an American Association for the Advancement of Science (AAAS) press release.
Researchers from Ankara City Hospital in Turkey highlighted that patients with Covid-19 also developed candidemia earlier than those without Covid-19—at about 2 weeks into ICU time—and died before receiving any antifungal treatment.
“Some of the remaining patients with Covid-19 were able to receive antifungal treatment for shorter than proper treatment duration. These results show that candidemia does not come to mind in the early period of infection in ICU patients, especially Covid-19 patients,” wrote Bircan Kayaaslan, MD, and co-authors in Mycoses.
And in related research, a group from Ludwig-Maximilians-University in Munich, Germany, evaluated the immune phenotype and cytokine release pattern of patients with both diseases, and offered the “first evidence of a disturbed immune response toward C. albicans, which may hint at an increased susceptibility toward infection with C. albicans in critically ill Covid-19 patients. We consider the immune response characterization of critical Covid-19 cases as relevant for the field, and the blunted cytokine response to stimulation with C. albicans noteworthy to both immunologists and clinicians,” they wrote in Frontiers in Immunology.
Karmarkar and co-authors noted that in 2018, a lab serving LTACHs in Southern California began pinpointing species of Candida in urine specimens to enhance surveillance of C. auris, which was then identified in February 2019 in a patient in an Orange County LTACH.
They wanted to assess the prevalence of C. auris and IPC practices in LTACHs (n=3) and vSNFs (n=14) in the county, and measured “antifungal susceptibility” and isolate relatedness with whole-genome sequencing (WGS).
The authors explained that in “facilities where C. auris was detected, PPSs were repeated every 2 weeks. Ongoing IPC support was provided,” after they determined that pre-intervention, hand hygiene rates at all facilities with C. auris were below 80%, and that there were multiple “gaps in environmental cleaning…and disinfection…At several facilities, staff responsibilities for cleaning computers, hospital carts, and bed alarms were unclear, and the frequency of cleaning of mobile medical equipment was unspecified.” They also noted that more than half the facilities did not have a chart labeling system to identify patients colonized with multidrug-resistant organisms.
For clinical outcomes, the authors found that, out of 182 patients with screening cases of C. auris, 8% were subsequently diagnosed with clinical cases, and 43% were diagnosed through urine. The first patient with a positive blood culture result was seen in May 2019 at a single LTACH. As of early 2020, of 12% of the patients died within 30 days of C. auris identification, and 26% died within 90 days, with a single death was attributed to C. auris.
Based on WGS, it was determined that Orange County isolates differed by 29 to 102 single nucleotide polymorphism (SNPs) from clade III strains previously reported in Indiana, Maryland, Kenya, South Africa, and the U.K, as well as being >1,000 SNPs different from clade III strains from Canada.
Finally, post-intervention for IPC gaps or ongoing transmission, repeat assessments demonstrated improved hand hygiene, along with “qualitative improvement in environmental cleaning at several facilities…By October 2019, only…22%…[of] facilities with C. auris identified on initial PPS…had ongoing transmission; both had the highest initial prevalence of C. auris, Karmarkar and co-authors stated.
Study limitations included the fact that the authors could not identify the Orange County “patient zero” with C. auris</em>; acute-care hospitals were not assessed; and the fact facility IPC practices could not be tracked over time. The authors acknowledged that “replicating this intensive investigation in regions with fewer resources, a larger population, or a more complex health care network may be challenging.”
Mody and Cassone called for “future research to [decipher] the most common chains of C. auris transmission, as well as establish integrated and cost-effective surveillance networks that harmonize sensible active screening with improved knowledge of clinical risk factors.”
UNIFESP and others are conducting a gene-sequencing study to get a better understanding of C. auris drug resistance. “The mechanism that enables the species to develop drug resistance isn’t enzymatic degradation, as in so many bacteria that are resistant to antibiotics,” Colombo stated in the AAAS press release.”If the analysis is conducted using conventional automated methods, C. auris can be confused with other species, such as C. haemulonii or C. lusitaniae.”
- Enhanced laboratory surveillance and prompt investigation with infection-and-prevention control (IPC) support resulted in rapid identification and containment of Candida auris in ventilator-capable skilled-nursing facilities and long-term acute care hospitals in Orange County, California.
- Assessments of IPC practices showed gaps in hand hygiene, transmission-based precautions, and environmental cleaning,” but post-intervention, the “outbreak was contained to two facilities in a matter of months.
Shalmali Pal, Contributing Writer, BreakingMED™
The study was supported by the CDC/CDC Combating Antibiotic Resistant Bacteria Initiative.
Karmarker reported no relationships relevant to the contents of this paper to disclose. Co-authors reported support from the CDC, the American Health Care Association, Society for Healthcare Epidemiologists of America, and the Infectious Disease Society of America.
Cat ID: 125
Topic ID: 79,125,287,292,503,728,791,730,125,190,469,520,192,151,925



Create Post
Twitter/X Preview
Logout