Implanting allogeneic modified bone marrow-derived mesenchymal stromal/stem cells in patients with traumatic brain injury (TBI) met efficacy and safety endpoints in an interim analysis from the phase II randomized controlled STEMTRA trial.
“This study provides Class I evidence that implantation of SB623 was well tolerated and associated with improvement in motor status,” wrote Masahito Kawabori, MD, PhD, of Hokkaido University in Sapporo, Japan, and co-authors, in Neurology.
The authors reported 6-month results for the 1-year sham-controlled trial of stereotactic implantation of cells called SB623 in 61 patients with stable chronic motor deficits due to TBI. Participants were randomized to sham injection (n=15) versus doses, in millions of cells, of 2.5, 5, or 10 (n=16 each). Motor function was assessed with the Fugl-Meyer Motor Scale scores (FMMS) summed to 100 maximum upper limb and lower limb points — higher scores imply better function and clinically meaningful change is considered 10 points. Baseline scores in both groups were about 52.
FMMS score improvement was 8.3 points for treated patients versus 2.3 points for controls (P=0.04). A clinically meaningful improvement of 10 or more FMMS points was seen in 39.1% of patients in the treatment arms versus 6.7% for controls (P=0.039). While 100% of treated patients and 93.3% of controls experienced treatment-related adverse effects, no dose-limiting toxicities or deaths were seen.
“In this trial a classical dose response was not seen, with patients in the SB623 5.0×106 treated group achieving the most favorable FMMS outcomes at 6 months,” the authors observed. “The SB623 10.0×106 cell dose did not confer additional benefit, and in general was associated with increased variability (i.e., a greater range in efficacy responses). We speculate that beyond a certain threshold the beneficial effects of additional cell implantation may be counterbalanced by locally increased inflammation secondary to increased cell death, or that a biological asymptote had been reached.”
In an accompanying editorial, Masha Savelieff, PhD, and Eva Feldman, MD, PhD, both of the University of Michigan in Ann Arbor, wrote that “STEMTRA used a targeted delivery of stem cells to the injury site, an approach further supported by the recent failed phase III clinical trial of non-targeted intrathecal injections in amyotrophic lateral sclerosis.”
Potential advantages of allogeneic bone marrow-derived mesenchymal stromal/stem cell implants include no requirement for concomitant immunosuppression, readily available cells free of ethical concerns, and low risk of malignant transformation, they pointed out.
“Therefore, in light of the lack of current TBI therapies, and if these positive findings hold at study conclusion, the results of this STEMTRA phase II trial would advocate a phase III trial,” they said.
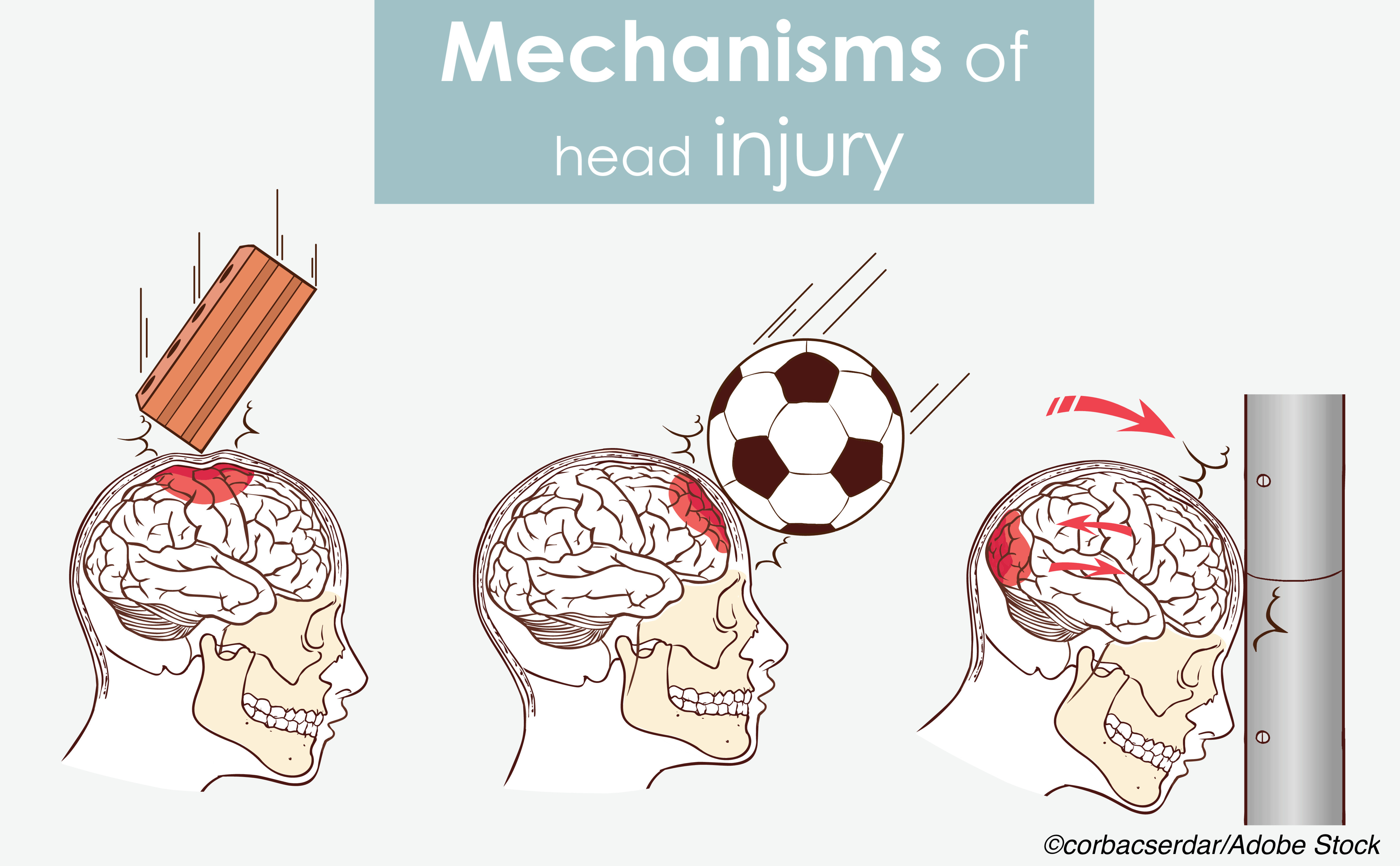
The acute physical injury causing TBI is followed by secondary damage involving inflammation, oxidative stress, and excitotoxicity. Treatment is guided by severity and limited options, and may include head elevation, hyperventilation, hyperosmolar therapy, seizure treatment, induced coma, and cooling. Intracranial pressure monitoring, decompressive craniotomy, and other surgical procedures are used as indicated.
No known treatments prevent or stop secondary damage, but cell-based therapy with goals of both neuroreplacement — as with implanted neural stem cells or treatments designed to bolster endogenous neural stem cells — and neurorestoration, through supportive mechanisms, has been an important area of research for several decades. Neurorestorative mechanisms for improvement involve neurogenesis, angiogenesis, and immunoregulation through chemokine and growth factors.
The present study used modified mesenchymal stem cells that expressed the intracellular domain of Notch-1 to give the cellular product SB623, Savelieff and Feldman explained. “Notch-1 expression prevents SB623 differentiation into bone, cartilage, or adipose cells, and boosts SB623 trophic and chemotactic factor expression and extracellular matrix deposition, which may nurture damaged brain cells in TBI.”
Kawabori and colleagues studied patients with moderate or severe TBI whose chronic motor defects were due to a focal brain lesion. Mean age was 34.4, and time since injury ranged from 1.4 to 28.4 years. Cells were placed stereotactically adjacent to the TBI lesion.
Nonsignificant differences were seen in secondary outcomes measuring global function and disability, as well as quality of life. These included the Disability Rating Scale, Action Research Arm Test, Gait Velocity, NeuroQOL upper and lower extremity scores, and Global Rating of Perceived Change.
The most frequent adverse event was headache in both the pooled treatment group (50.0%) and the control group (26.7%; P=0.14); more than 90% in both groups were mild or moderate in severity. No significant differences were seen in the frequency of adverse events between groups.
Serious adverse events were seen in six patients overall: 8.7% of the treatment group (n=4: delirium, sensory change/TIA, seizure, and delirium/balance worsening) and 13.3% of controls (n=2: wound infection, fall from bicycle).
“The vast majority of treatment emergent adverse effects were unrelated or unlikely to be related to cell treatment, while in common with previous studies, many treatment emergent adverse effects were possibly, probably, or definitely related to surgical procedure,” Kawabori and co-authors wrote.
No relationship was seen between the presence of anti-SB623 HLA antibodies and cell dose, incidence of serious adverse events, or efficacy parameters.
“The STEMTRA studies are shedding light on a potential stem cell ’neighborhood theory,’ where stem cells may exert a salutary effect by nurturing and supporting injured neurons and glia,” the editorialists noted. Future research in the area should address whether treatment improves global functional outcomes, include cognitive tests to avoid masking motor improvements, standardize evaluation criteria for implanted stem cell efficacy, and further explore dose related benefits, they suggested.
Limitations include response to treatment that may have been variably influenced by lesion location.
-
Implanting allogeneic modified bone marrow-derived mesenchymal stromal/stem cells in patients with traumatic brain injury (TBI) met efficacy and safety endpoints in an interim analysis from the phase II STEMTRA trial.
-
This study provides Class I evidence that implantation of stereotactic implantation of cells called SB623 was well tolerated and associated with improvement in motor status.
Paul Smyth, MD, Contributing Writer, BreakingMED™
This study was sponsored by SanBio, Inc.
Kawabori is a consultant for SanBio.
Feldman reports personal fees from Novartis, outside the submitted work.
Cat ID: 130
Topic ID: 82,130,730,130,474,192,925



Create Post
Twitter/X Preview
Logout