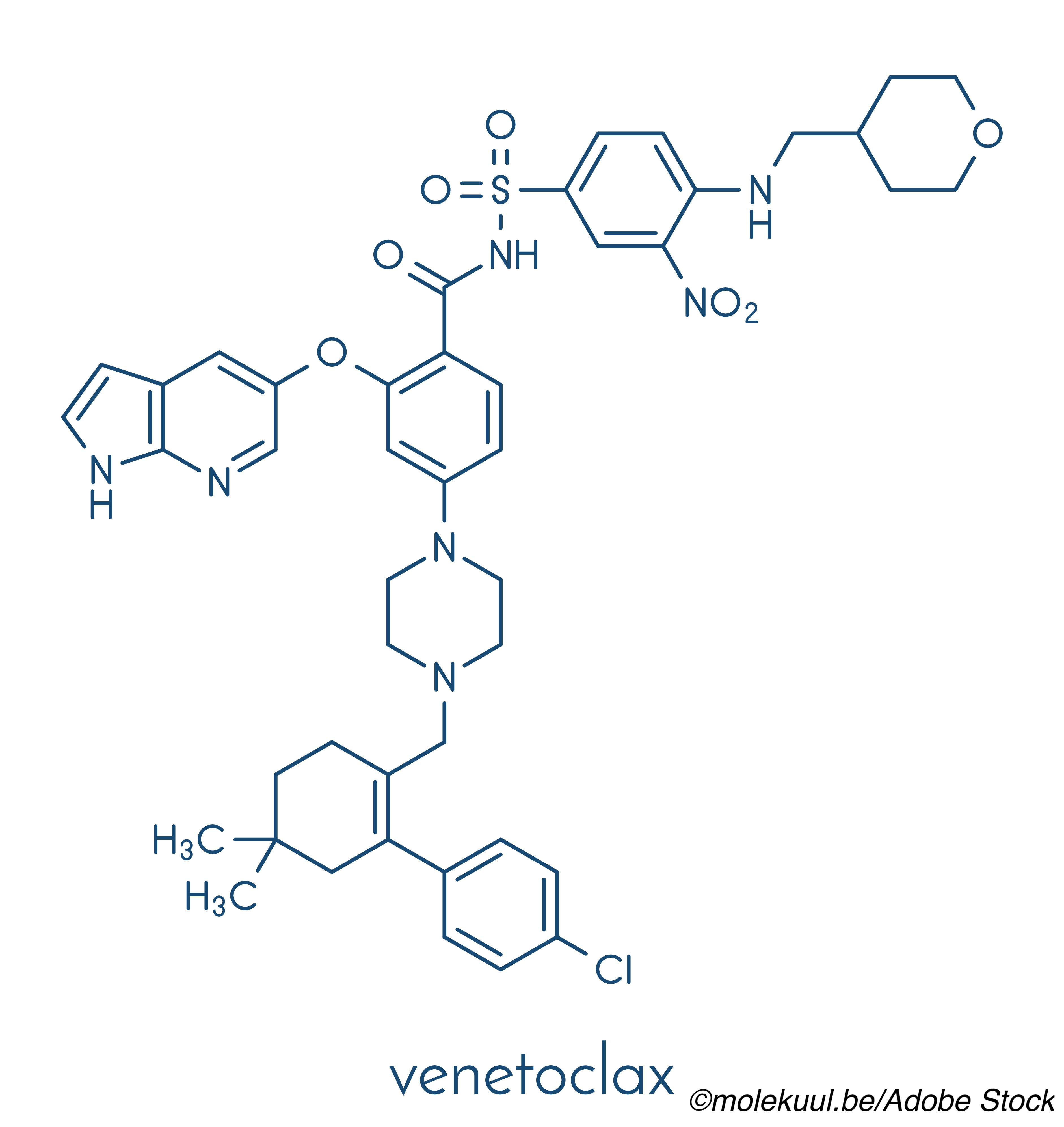
The FDA granted full approval to venetoclax (Venclexta) to treat newly-diagnosed acute myeloid leukemia (AML) in adults 75 years of age or older with comorbidities that prevent them from receiving intensive induction chemotherapy.
The agency first granted venetoclax accelerated approval for this indication in 2018, contingent upon verification of the BCL-inhibitor’s clinical benefit through confirmatory trials. That extra confirmation came in the form of data from the phase III VIALE-A and VIALE-C studies, the drug’s manufacturer, AbbVie, announced in a company press release.
In the VIALE-A trial, which was presented as a late breaker at the June 2020 European Hematology Association (EHA) Annual Congress and recently published in the New England Journal of Medicine, “patients on the active regimen of [venetoclax] plus azacitidine achieved a 34% reduction in the risk of death compared to azacitidine in combination with placebo (Hazard Ratio [HR]=0.66 [95% CI: 0.52-0.85], P<0.001),” the company wrote. “The median OS for patients in the [venetoclax] arm was 14.7 months (95% CI: 11.9, 18.7) versus 9.6 months in the placebo arm (95% CI: 7.4, 12.7). Additionally, patients in the [venetoclax] plus azacitidine arm achieved a complete remission (CR) rate of 37% (95% CI: 31%, 43%) with a median duration of CR of 18.0 months (95% CI: 15.3, -) compared with patients in the placebo plus azacitidine arm with a CR rate of 18% (95% CI: 12%, 25%) with a median duration of CR of 13.4 months (95% CI: 8.7, 17.6). The observed safety profile was generally consistent with the known safety profile of [venetoclax] in combination with azacitidine. For patients taking [venetoclax] in combination with azacitidine, the most frequent serious adverse reactions (ARs; ≥5%) at first use were febrile neutropenia (30%), pneumonia (22%), sepsis (excluding fungal; 19%) and hemorrhage (6%).”
As for the VIALE-C trial, which was presented both the EHA Congress and the 2020 American Society of Clinical Oncology (ASCO) meeting and published in Blood, “The median OS for [venetoclax] in combination with LDAC was 7.2 months (95% CI: 5.6, 10.1) and 4.1 months for LDAC in combination with placebo (95% CI: 3.1, 8.8). The HR for the primary endpoint of OS was 0.75 (95% CI: 0.52-1.07; p=0.114). The trial did not meet its primary endpoint of statistically significant improvement of OS for patients with AML who are ineligible for intensive chemotherapy at the time of the planned analysis. Efficacy was based on the rate of CR and duration of CR with supportive evidence of rate of CR + complete remission with partial hematologic recovery (CR+CRh), duration of CR+CRh, and the rate of conversion from transfusion dependence to transfusion independence. In the [venetoclax] arm, the most frequent serious ARs were (≥10%) pneumonia (17%), febrile neutropenia (16%) and sepsis (excluding fungal; 12%).”
“For far too long, people with AML had very few treatment options, aside from very intense chemotherapy, said Lee Greenberger, PhD, chief scientific officer of The Leukemia & Lymphoma Society, in a statement. “Today’s news continues the progress of bringing more treatment options to patients with this devastating disease.”
The most common adverse events associated with use of venetoclax for AML included nausea, diarrhea, thrombocytopenia, constipation, neutropenia, febrile neutropenia, fatigue, vomiting, edema, pyrexia, pneumonia, dyspnea, hemorrhage, anemia, rash, abdominal pain, sepsis, musculoskeletal pain, dizziness, cough, oropharyngeal pain, and hypotension. The drug’s prescribing information also includes a warning for tumor lysis syndrome (TLS), advising physicians to test patients for TLS risk prior to beginning treatment and adivising patients to stay hydrated over the course of treatment and notify their health care professional if they experience fever, chills, nausea, vomiting, confusion, shortness of breath, seizures, irregular heartbeat, dark or cloudy urine, unusual fatigue, or muscle or joint pain, as these may be symptoms of TLS.
Venetoclax also carries warnings for neutropenia and an increased risk for infections.
John McKenna, Associate Editor, BreakingMED™
Cat ID: 466
Topic ID: 78,466,730,466,192,725,925