When present with sporadic cerebral cavernous malformations (CCMs), developmental venous anomalies (DVAs) did not influence intracranial hemorrhage (ICH) risk or, when bleeding did occur, ICH size, an observational study found.
While the risk of first or further hemorrhage with CCM at 5 years was 24.1% (95% CI 21.1%–27.5%), patients who presented with hemorrhage were less likely to have associated DVA (OR 0.635; 95% CI 0.459–0.878), reported Bixia Chen, MD, of the University of Duisburg-Essen in Germany, and coauthors.
Independent predictors of first or recurrent hemorrhage with CCM were first presentation as ICH (HR 8.0; 95% CI 3.549–18.122) and brainstem as site of the malformation (HR 2.9; 95% CI 1.756–4.765), they wrote in Neurology. The association for DVA was nonsignificant (HR 1.1; 95% CI 0.717–1.885).
Hemorrhage volumes of >5 ml, >20 ml, and >30 ml showed no correlation with DVA, and no difference in mean ICH size for groups with and without associated DVA.
“Associated DVAs do not correlate with higher hemorrhage risk of CCMs or more severe bleedings,” Chen and collaborators wrote. “In this cohort, bleeding risk was even lower in patients with DVAs.
“In accordance with other CCM studies, patients with brainstem localization showed an increased risk to present with a hemorrhage, and initial ICH and brainstem localization were baseline predictors for a (re)hemorrhage during follow-up,” they added. “Our results are important for patient counseling.”
In an accompanying editorial, Alejandro Rabinstein, MD, and Kelly Flemming, MD, both of the Mayo Clinic in Rochester, Minnesota, wrote that the study “probably provides the best available data on the risk of hemorrhage in radiographic apparent DVA-associated sporadic CCMs. These results have direct clinical implications in that they indicate that the presence of a DVA should not be considered an argument to support surgical treatment of the CM.”
“This study is particularly important because previous findings in some smaller cohorts suggested a higher risk of bleeding when the CCM was associated with a DVA, although others also found the bleeding risk to be the same or lower,” they added. “The substantially larger size of the cohort in the study by Chen et al. makes its results more credible.”
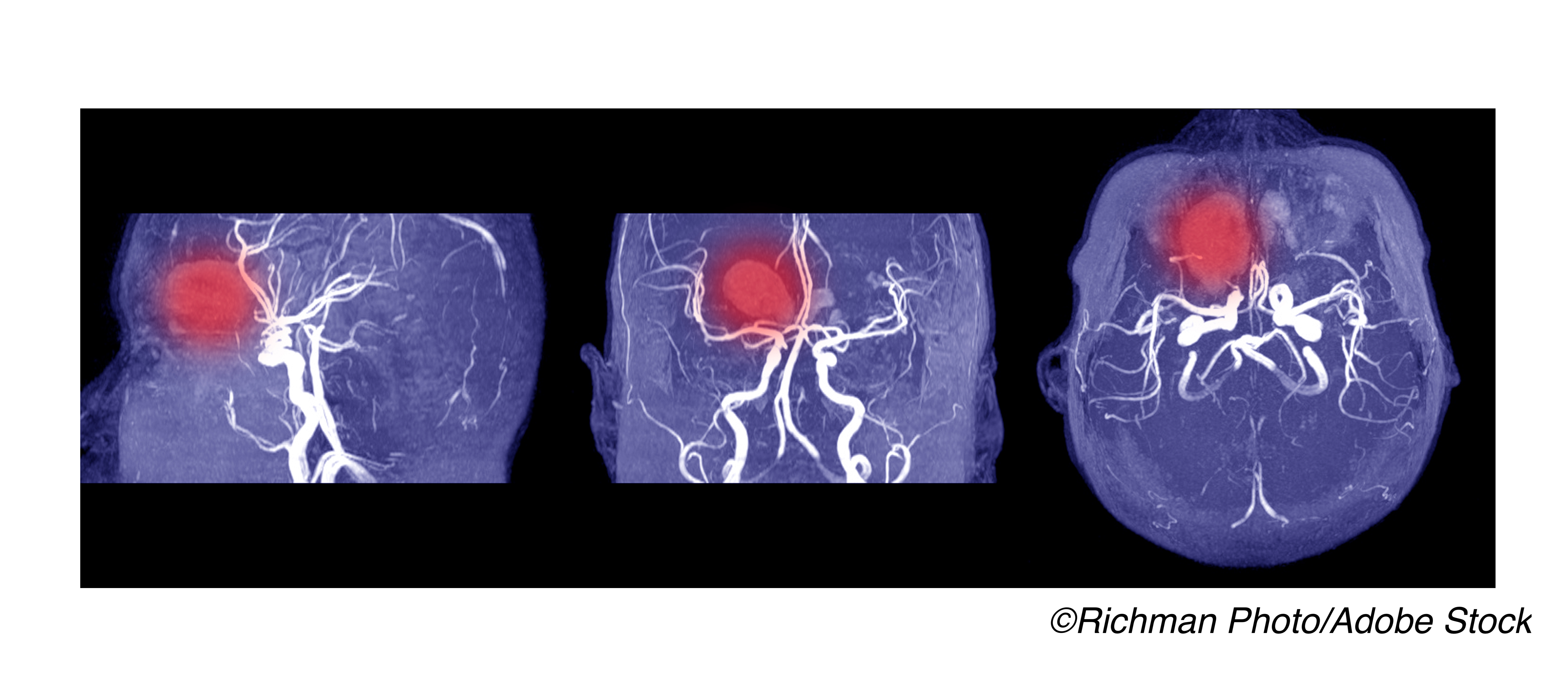
CCMs are vascular cavities lined by endothelial cells without tight junctions. Though suggestive signs such as microcalcifications may be seen on CT, they are not definitive. CCMs are also not detected on angiography, so MRI is used to diagnose and monitor CCMs for increase in size or possible bleeding.
CCMs may be familial or sporadic. Familial cases — often with multiple sites, and associated with genes CCM1, CCM2, and CCM3 — have been combined with sporadic cases in some prior research, though they may have different origins and natural histories.
CCMs also be may be asymptomatic or present with hemorrhage, seizure, or focal neurologic deficits. A prior study of CCM found that increased risk of 5-year symptomatic hemorrhage was associated with brainstem location of CCM and with presentation of either ICH or focal neurologic deficit when imaging did not suggest recent bleeding.
On 1.5T MRI, about a quarter of sporadic CCMs are accompanied by DVA—dilated venous vessels that converge in a radial pattern to an enlarged collecting vein. With higher sensitivity imaging (7T MRI), an even larger percentage is likely, though there may be structural variation compared to typical DVA.
“Sporadic CCMs without radiographically apparent DVA may still have local venous drainage abnormalities,” the editorialists explained. “Hemodynamic features related to venous drainage not only may contribute to the formation of CCMs but also may influence their subsequent risk of hemorrhage in ways that are yet undefined.”
DVAs are rarely symptomatic themselves, but there has been debate whether DVAs contribute to the formation of sporadic CCMs through hemodynamic and other mechanisms.
Guidelines for management suggest nonsurgical monitoring of asymptomatic CCM cases and surgical intervention constrained by lesion severity, progression, and associated symptoms in some. Important questions remain, though, about the presence of DVA with CM and implications for treatment: A CCM with DVA may pose additional bleeding risk over time, but also increase the risk of surgical treatment.
Prior studies on the effect of DVA on the risk of bleeding with CCM are inconsistent. For example, a 2014 analysis of 326 patients with CCM found no significant association of higher hemorrhage rate for those with associated venous malformation, while a 2018 study of 154 patients with CCM found that DVA conferred a higher risk of bleeding.
Chen and colleagues studied 731 patients with sporadic cerebral CCMs at their institution diagnosed with contrast-enhanced MRI between January 2003 and December 2018. Mean age was 41 and 61% were female. Associated DVA was present in 283 (38.7%). Follow-up was 5 years with a 64% completion rate.
About half overall presented with symptomatic ICH, and the cumulative 5-year risk for symptomatic ICH was 24.1%. Subgroup analysis showed no difference between DVA and no DVA groups, with 5-year ICH risks of 20.7% and 22.5%, respectively.
Limitations include the study’s 5-year follow-up rate of 64%. The authors also noted that patients with DVA are more prone to be diagnosed in the asymptomatic phase compared with patients with CCMs alone due to better visibility on brain imaging, which could favor a negative association with bleeding presentation.
- When present with sporadic cerebral cavernous malformations (CCMs), developmental venous anomalies (DVAs) did not influence intracranial hemorrhage (ICH) risk or, when bleeding did occur, ICH size, an observational study found.
- These results have direct clinical implications: the presence of a DVA should not be considered an argument to support surgical treatment of the CM, the editorialists wrote.
Paul Smyth, MD, Contributing Writer, BreakingMED™
No targeted funding reported.
The researchers report no relevant disclosures. The editorialists report no relevant disclosures.
Cat ID: 130
Topic ID: 82,130,130,192,925