The prolonged use of potent topical corticosteroids can increase the risk of osteoporosis and major osteoporotic fracture, Danish researchers found.
Alexander Egeberg, MD, PhD, Department of Dermatology and Allergy, Herlev and Gentofte Hospital, University of Copenhagen, and colleagues suggested that corticosteroid-sparing therapies should be considered for persons who require prolonged anti-inflammatory treatments on large areas of their bodies. Their study was published in JAMA Dermatology.
Long-term use of potent topical corticosteroids (TCSs) is common in patient with psoriasis, atopic dermatitis, and other inflammatory diseases. And, according to the authors, systemic effects can be seen with extreme use of these drugs, including striae formation (stretch marks), adrenal suppression, Cushing syndrome, and Addison crisis after quick withdrawal.
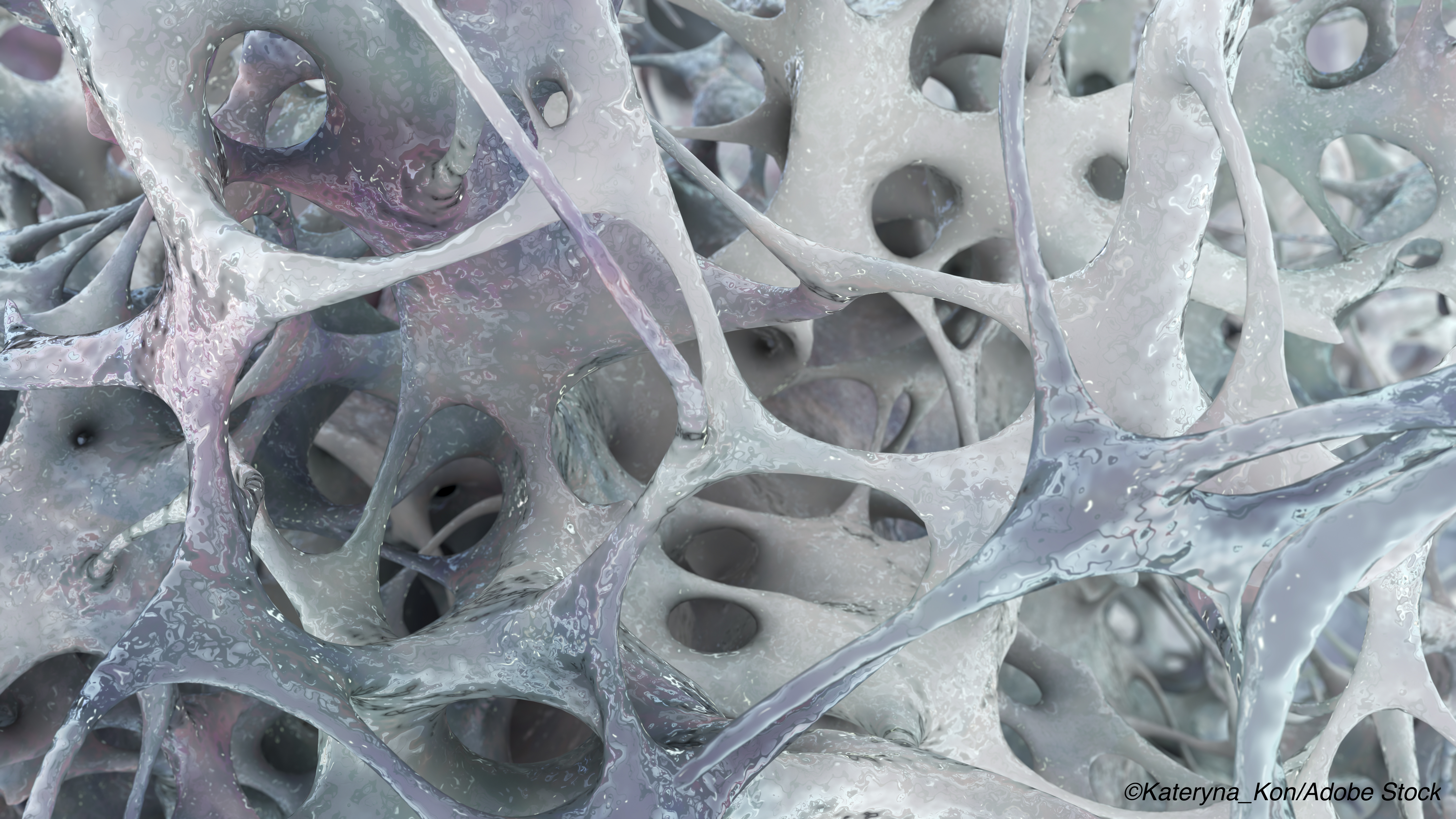
They can also negatively affect bone remodeling, leading to questions regarding the extent to which the prolonged use of topical corticosteroids increases the risk of osteoporosis and major osteoporotic fracture (MOF). Furthermore, according to Egeberg and colleagues, it is important to be able to quantify the effect of cumulative use of these topical agents on the risk of osteoporosis and MOF in order to better support patient treatment decisions.
In this nationwide retrospective cohort study, the authors used Danish national registries to gather data on 723,251 Danish adults treated with potent or very potent TCSs from Jan. 1, 2003, through Dec. 31, 2017.
Potent TCSs, such as mometasone furoate and betamethasone 17 valerate, and very potent TCSs, such as clobetasol propionate, were included in the study. Filled prescription data were converted in equally potent doses to mometasone furoate (1 mg/g) and person-time exposure to either drugs was divided into these categories: 200 to 499 g (reference group/unexposed), 500 to 999 g, 1,000 to 1,999 g, 2,000 to 9,999 g, and at least 10,000 g.
The incidence rate of osteoporosis in those given equivalent doses of mometasone was:
- 36.7 (95% CI, 36.0-37.4) per 10,000 person-years for 200 to 499 g.
- 43.1 (95% CI, 42.1-44.2) per 10,000 person-years for 500 to 999 g.
- 50.2 (95% CI, 48.7-51.7) per 10,000 person-years for 1,000 to 1,999 g.
- 55.2 (95% CI, 53.6-57.0) per 10,000 person-years for 2,000 to 9,999 g.
- 58.7 (95% CI, 53.8-64.1) per 10,000 person years for at least 10,000 g.
The incidence rate of MOF was:
- 81.6 (95% CI, 80.6-82.7) per 10,000 person-years for 200 to 499 g.
- 88.7 (95% CI, 87.2- 90.2) per 10,000 person-years for 500 to 999 g.
- 100.6 (95% CI, 98.4-102.8) per 10,000 person-years for 1,000 to 1,999 g.
- 113.1 (95% CI, 110.5-115.7) per 10,000 person-years for 2,000 to 9,999 g.
- 122.3 (95% CI, 115.0-130.1) per 10,000 person-years for at least 10,000 g.
In adjusted analysis, the authors determined that there was significant association between exposure to TCSs (any exposure ≥500 g versus 200-499 g) and the risk of osteoporosis (HR, 1.08; 95% CI, 1.05-1.11) and MOF (HR, 1.05; 95% CI, 1.03-1.07).
Egeberg and colleagues observed that there was a dose-response association between the increased use of potent or very potent TCSs and the risk of osteoporosis and MOF, with a 3% relative risk increase of osteoporosis and MOF per the doubling of the cumulative TCS dose (HR, 1.03 [95% CI, 1.02-1.04] for both).
The authors also found that the population-attributable risk of any exposure compared with nonexposed individuals was 4.3% (95% CI, 2.7%-5.8%) for osteoporosis, and 2.7% (95% CI, 1.7%- 3.8%) for MOF. This suggests, they wrote, that 4.3% of osteoporosis cases and 2.7% of fractures could have been prevented if patients had used other therapies instead of potent TCSs. However, they added that the absolute risk for individual patient was low
They also suggested that while alternatives to potent TCS treatments on large body surfaces of patients might limit the risk of osteoporosis, these patients could also consider earlier evaluation of and prophylaxis for osteoporosis and prophylactic therapy.
In an editorial accompanying the study, Rebecca D. Jackson, MD, The Ohio State University, Columbus, noted that the study does not suggest that topical TCSs administered in conventional doses cause considerable harm, and does not determine whether the risk of osteoporosis or fracture differs by underlying disease and disease severity. She also noted that absorption of TCSs can differ according to body location, surface area covered, and skin integrity — all of which can influence risk.
To manage risk “it would be prudent to select a TCS regimen that reflects the lowest dose for the shortest duration necessary to manage the underlying medical condition,” Jackson suggested, adding that when the dose approaches the highest thresholds non–glucocorticoid-based treatments could be considered to improve patient outcomes.
-
Prolonged use of potent topical corticosteroids increases the risk of osteoporosis and major osteoporotic fracture.
-
Corticosteroid-sparing therapy may need to be considered in cases where patients require potent anti-inflammatory treatments on large surface areas of the body for extended periods.
Michael Bassett, Contributing Writer, BreakingMED™
Egeberg reported receiving grants, personal fees, and nonfinancial support from Pfizer, Inc, Eli Lilly and Company, Novartis International AG, and UCB; grants from Janssen Pharmaceutica; grants and personal fees from AbbVie and Bristol Myers Squibb; personal fees from Dermavant Sciences, Almirall SA, Leo Pharma A/S, Samsung Bioepis Co, Ltd, Galderma SA, Janssen Pharmaceutica, Sun Pharmaceutical Industries Ltd, and Galapagos NV; and research funding from the Danish National Psoriasis Foundation outside the submitted work.
Cat ID: 105
Topic ID: 75,105,105,109,15,192,158,925