Implementation of the federally mandated sepsis management bundle SEP-1 was associated with substantial changes in sepsis resuscitation care but no significant improvement in clinical outcomes, according to results from a study involving more than 50,000 patients treated at 11 U.S. hospitals from 2013 through 2017.
Instituting the SEP-1 bundle was associated with a 50% increase in lactate checks, a 10% increase in the administration of broad-spectrum antibiotics, and a 30% increase in infusions of 30 mL/kg of intravenous fluid within three hours of culture order at 11 University of Pittsburgh Medical Center (UPMC)-affiliated hospitals.
Despite this increase in patient management, no significant changes were reported in hospital mortality or the percentage of patients discharged to home in the longitudinal study, which was funded by the Agency for Healthcare Research and Quality (AHRQ).
The study findings were published online April 19 in Annals of Internal Medicine.
Researcher Ian Barbash, MD, of the UPMC Montefiore Hospital, and colleagues wrote that while the findings confirm that pay-for-reporting programs can influence bedside care in the critical care setting, “the overall effect was modest and largely limited to the elements of SEP-1 with indirect effect on patient outcomes (lactate measurement), rather than the element most tightly linked to better outcomes (early antibiotics).”
They added that the findings “raise questions about the value of SEP-1.”
“Hospitals are investing tremendous time and energy in responding to SEP-1, including many hours of data abstraction,” they wrote. “Indeed, one cost analysis suggested that a single academic hospital invested more than $150,000 per month in the SEP-1 response. If SEP-1 incentivized hospitals to dedicate quality improvement resources to increasing adherence with processes that did not improve survival, it may have failed to achieve its intended goal.”
The Centers for Medicare & Medicaid Services (CMS) implemented SEP-1 in October of 2015, and the policy remains controversial.
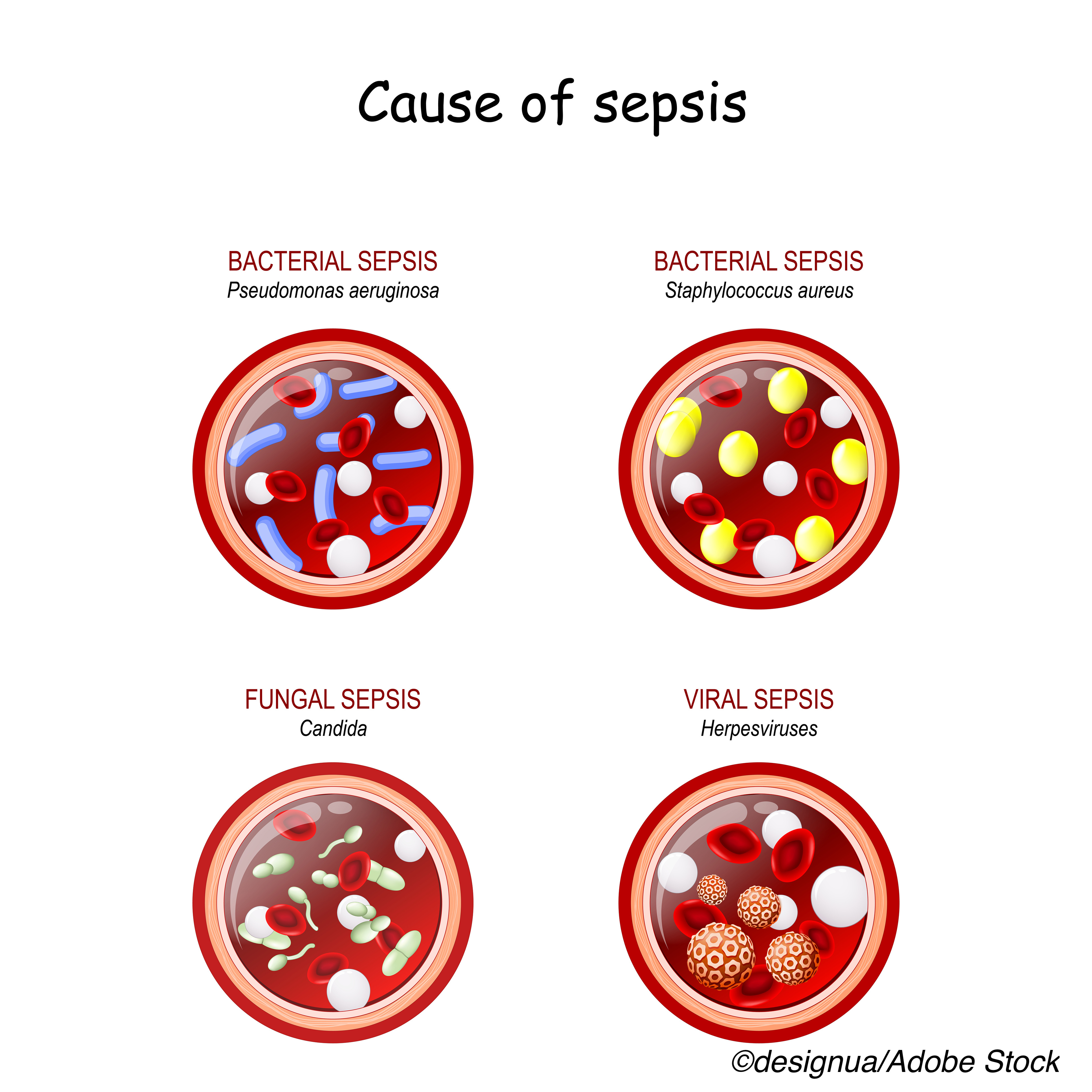
The program requires hospitals to report adherence to sepsis-management measures including obtaining blood cultures, checking serum lactate levels, administration of broad-spectrum antibiotics and fluid administration within three hours of sepsis onset. The bundle also mandates starting vasopressors for persistent hypotension and documenting a repeated volume status examination within six hours.
In commentary published with the study, Michael Klompas, MD and Chanu Rhee, MD, of Harvard Medical School/Brigham and Women’s Hospital, Boston, wrote that while proponents of SEP-1 contend that the bundle has brought “welcome attention to sepsis and catalyzed hospital to implement protocols that save lives,” critics counter that the program’s “rigid treatment requirements and aggressive timelines” have led to overtreatment and unnecessary burdens on health care provider time.
“Critics have also questioned the evidence supporting SEP-1,” they wrote. “Supporters point to observational studies that report lower mortality rates after implementing sepsis bundles. However, these studies are difficult to interpret because bundle implementations are inevitably accompanied by awareness campaigns that increase the detection of milder cases of sepsis.”
In their study, Barbash and colleagues evaluated data from electronic health records to determine the effect of SEP-1 on patient management and risk-adjusted outcomes.
Using repeated cross-sectional patient cohorts, the researchers evaluated changes in specific SEP-1 targeted strategies, including antibiotic administration, lactate measurement and fluid administration within three hours of sepsis onset, repeated lactate and vasopressor administration for hypotension within six hours, and sepsis outcomes.
The analysis revealed that two years after its implementation, SEP-1 was associated with variable changes in process measures, with the greatest effect being an increase in lactate measurement within three hours of sepsis onset (absolute increase, 23.7 percentage points; 95% CI, 20.7-26.7 percentage points; P<0.001).
Among the other main findings:
- Small increases in antibiotic administration were reported (absolute increase, 4.7 percentage points; 95 % CI, 1.9-7.6 percentage points]; P=0.001).
- Administration of fluid 30 mL/kg of body weight within three hours of sepsis onset also increased (absolute increase, 3.4 percentage points; 95% CI, 1.5-5.2 percentage points; P<0.001).
- No change was reported in vasopressor administration.
- There was a small increase in ICU admissions (absolute increase, 2.0 percentage points, 95% CI, 0-4.0 percentage points; P=0.055) and no changes in mortality (absolute change, 0.1 percentage points; 95% CI, −0.9 to 1.1 percentage points; P=0.87) or discharge to home.
Potential study limitations cited by the researchers included defining time of suspected infection as the time of sepsis onset in their primary analysis.
“The issue of sepsis time zero is controversial and without a gold standard,” they wrote, adding that the finding of similar results in sensitivity analysis calculating time of sepsis onset as time from ED arrival was reassuring. The fact that the data came from a single health system and the relatively low overall mortality increased the possibility that the patients were not sick enough to benefit from small increases in the quality of care, the researchers noted.
Klompas and Rhee added that the UPMC health system is recognized as a leader in emergency and critical care medicine.
“Results from this hospital system may not be generalizable to other organizations,” they wrote, noting that additional research is needed “to evaluate the effect of SEP-1 across a broader array of hospitals.”
“What then is the way forward for SEP-1 and the still critical goal of improving sepsis care? We think there are two simultaneous paths to follow,” they wrote.
Their first recommendation is the establishment of better diagnostics to identify infection, determine cause and antimicrobial susceptibility, and inform real-time antibiotic selection.
“This is not a pipe dream,” they wrote. “We already have rapid and accurate molecular diagnostic tools for many respiratory viruses and selected bacterial pathogens. Fostering the development of improved diagnostic including susceptibilities, nurturing studies on their effects on outcomes, and facilitating their deployment are tangible ways that governments and foundations can advance sepsis care.”
Their second recommendation involved the shift of sepsis reporting away from “debatable process measures and onto objective outcomes using standardized, clinically meaningful, electronically definable, risk-adjusted indicators.”
“This will help avoid the risk for therapeutic misdirection inherent in mandating overly rigid bundles; respect the physician’s art in weighing diagnostic likelihoods with the risks and benefits of potential treatments; and allow clinicians and hospitals room to innovate new ways to improve sepsis recognition, tailor sepsis care, and improve outcomes,” they concluded.
-
Implementation of the federally mandated sepsis management bundle SEP-1 was associated with substantial changes in sepsis resuscitation care but no significant improvement in clinical outcomes.
-
Despite this increase in patient management, no significant changes were reported in hospital mortality or the percentage of patients discharged to home in the longitudinal study.
Salynn Boyles, Contributing Writer, BreakingMED™
This research was funded by the Agency for Healthcare Research and Quality.
Babash reported grants from Agency for Healthcare Research and Quality, during the conduct of the study and from UPMC Health System, outside the submitted work.
Klompas and Rhee disclosed no relevant relationships.
Cat ID: 500
Topic ID: 498,500,500,503,728,791,730,125,190,469,520,192,463,925


Create Post
Twitter/X Preview
Logout