A study by Danish researchers suggests that a coronary artery calcium (CAC) score of 0 may not be a reliable marker for diagnosing obstructive coronary artery disease (CAD) in symptomatic individuals age 40 or younger, according to findings published in JAMA Cardiology.
Moreover, at any age, individuals diagnosed with CAD who had a CAC score of 0 appear to have an increased risk of myocardial infarction (MI) and all-cause death.
“These results showed that the diagnostic value of a CAC score of 0 beyond clinical variables in symptomatic patients was not uniform across age groups. To identify obstructive CAD in symptomatic younger patients and in women, an approach involving coronary computed tomography angiography (CCTA) is needed despite a CAC score of 0,” wrote Martin Bødtker Mortensen, MD, PhD, of Aarhus University Hospital, Denmark, and colleagues.
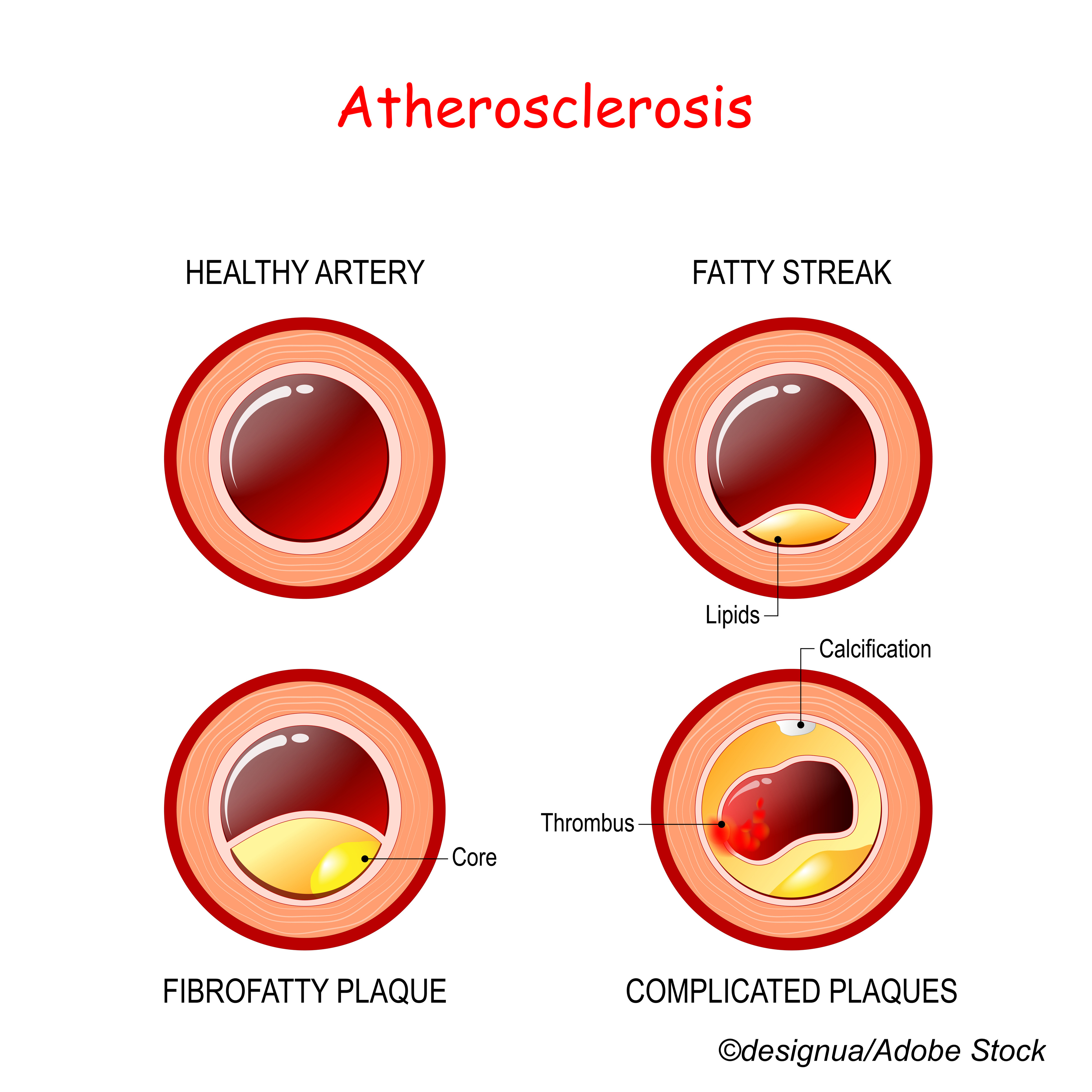
CAC testing consists of CT scans to assess calcium buildups in plaques located on the walls of the coronary arteries. The higher the CAC score, the higher the chance of significant coronary artery narrowing and the higher the risk for future cardiovascular events such as MI.
In an e-mail correspondence, Mortensen explained the rationale behind the study to BreakingMED: “Patients with stable chest pain are a very frequent problem in daily clinical practice. We know that many have non-cardiac causes for their symptoms. Thus, there is a great interest in identifying tools that can easily and reliably be used to rule out obstructive CAD in symptomatic patients.”
He and his colleagues undertook this study to assess the diagnostic value of a CAC of 0 in ruling out obstructive CAD in different age groups. They used data from the Western Denmark Heart Registry to identify 23,759 patients aged 18 and older who had computed tomography angiography (CTA) between Jan. 1, 2008, and Dec. 31, 2017, for symptoms suggesting CAD. Of these patients, 12,771 (54%) had a CAC score of 0 and comprised the study cohort.
They defined obstructive CAD as 50% or more luminal stenosis, and the main outcome of the study was the percentage of patients with obstructive CAD with a CAC score of 0. Median patient age was 58 years, and 55% were women.
CAD was found in 5,043 patients, and its prevalence across all age groups was low, ranging from 3% in those ˂40 years to 8% in those ≥70 years.
In all, 14% of patients with obstructive CAD had a CAC score of 0, with its prevalence ranging from 58% in those less than 40 years of age to 34% in those ages 40-49 years, 18% in those ages 50-59, 9% in those ages 60-69, and 5% in those ≥70.
Mortensen and colleagues found that the added diagnostic value of a CAC of 0 decreased at younger ages. In patients less than 40 years old, the risk factor-adjusted diagnostic likelihood ratio of a CAC of 0 was 0.68—a 32% lower-than-expected likelihood of obstructive CAD. In patients ≥70, it was 0.18, which translated to a roughly 82% lower-than-expected likelihood of obstructive CAD.
Upon comparisons of obstructive and nonobstructive CAD in patients with a CAC score of 0, researchers found associations with myocardial infarction and all-cause death (multivariable adjusted hazard ratio [HR] of 1.51; 95% CI: 0.98-2.33). This association differed, however, in younger patients ˂60 years old (adjusted HR: 1.80; 95% CI: 1.02-3.19) compared with those ≥60 (adjusted HR: 1.24; 95% CI: 0.64-2.39).
Over a median of 4.3 years of follow-up, 774 first-time MI or all-cause deaths occurred, of which 31% were in patients with a CAC score of 0.
“Although patients with CAC=0 are at low risk for having obstructive CAD (both young and older patients), it is important to realize that a large proportion of obstructive CAD in younger patients occur among those with CAC=0. Thus, an approach using CCTA is needed to identify most obstructive CAD at younger ages. Importantly, however, patients with CAC=0 have a good prognosis with an annual event rate <1% irrespectively of whether there is stenosis or not. This demonstrates the great prognostic value of CAC=0,” Mortensen noted, adding that in Denmark, a CAC scan is done just before CCTA, and is rarely performed alone.
“It is important for physicians to distinguish between the diagnostic and prognostic value of CAC in the setting of chest pain patients and why we do the diagnostic tests. If patients have stable chest pain, they may derive symptomatic benefit from revascularization if they have obstructive CAD found to be hemodynamically significant. For long-term prognosis, however, it is primary the burden of disease that defines risk. Our data are completely in line with this,” he concluded.
In an accompanying editorial, Sadiya S. Khan, MD, MSc, and Ann Marie Navar, MD, PhD, noted:
“Among asymptomatic middle-aged to older adults, one of the most sensitive, reliable, and reproducible ways of noninvasively identifying subclinical atherosclerosis is coronary artery calcium (CAC) testing. Numerous studies have demonstrated the robust association between presence and severity of CAC and future risk of cardiovascular disease (CVD). Conversely, the absence of CAC has been associated with low rates of CVD.”
They added: “When CAC is absent, current American Heart Association/American College of Cardiology guidelines recommend that clinicians consider providing no statin to some patients who are not at an elevated risk on the basis of smoking status, family history, and diabetes. Beyond this recommendation, however, some investigators have called for even more aggressive de-risking of patients with a CAC score of 0, suggesting that even those with familial hypercholesterolemia and a CAC score of 0 may not need statins. The article by Mortensen et al in this issue of JAMA Cardiology should give pause to efforts to broaden the use of a CAC score of 0 to de-escalate or defer statin therapy in all individuals.”
Khan, of Northwestern University Feinberg School of Medicine in Chicago, is JAMA Cardiology web editor, and Navar, of UT Southwestern Medical School in Dallas, is an associated editor of JAMA Cardiology. They added that these findings from Mortensen et al are in line with previous studies that have shown that most coronary plaques are noncalcified in younger patients and in women.
“Coronary artery calcium scoring is an excellent tool for identifying adults at a high risk for CVD, but caution should be exercised when translating the absence of CAC into delaying primary preventive interventions in younger adults and women. The goal of primary prevention should be to prevent the atherosclerotic lesions that lead to CAC, not to wait for CAC to develop before initiating risk-lowering therapy. Emphasizing true primary prevention of atherosclerosis before evidence of subclinical atherosclerosis emerges is of paramount importance to improve population-level cardiovascular health and to mitigate the growing burden of CVD morbidity and mortality,” they concluded.
Study limitations include possible referral and selection bias, the low risk of CAD in this European patient population, and nonadjustment of estimates for the potential implications of post-CTA management.
-
The diagnostic value of a coronary artery calcium (CAC) score of 0 to rule out obstructive coronary artery disease (CAD) was highly dependent on age.
-
A CAC score of 0 was associated with a substantial reduction in the likelihood of obstructive CAD in older patients, but the diagnostic value of a CAC score of 0 was smaller in younger patients.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This study was supported by public funding from Aarhus University Hospital.
Mortensen reported no disclosures.
Khan reported receiving grants from the American Heart Association and the National Institutes of Health outside the submitted work and being web editor for JAMA Cardiology.
Navar reported receiving grants from Bristol Myers Squibb, Esperion, Amgen, and Janssen; receiving personal fees from Amarin, Amgen, AstraZeneca, Boehringer Ingelheim, CSL, Esperion, Janssen, Lilly, Sanofi, Regeneron, Novo Nordisk, Novartis, The Medicines Company, New Amsterdam, Cerner, 89bio, and Pfizer outside the submitted work; and being associate editor for JAMA Cardiology.
Cat ID: 308
Topic ID: 74,308,730,308,192,925,481,96



Create Post
Twitter/X Preview
Logout