Immediate coronary angiography after successful resuscitation for out-of-hospital cardiac arrest (OHCA) without ST elevation showed no all-cause 30-day mortality benefit versus delayed angiography in the open-label TOMAHAWK trial.
The rate of all-cause 30-day mortality did not differ between the immediate and delayed groups (54.0% versus 46.0%, respectively; HR 1.28, 95% CI 1.00-1.63) in the primary intention-to-treat analysis, reported Steffen Desch, MD, of University of Leipzig in Germany, and co-authors in The New England Journal of Medicine.
A majority of patients died from severe anoxic brain injury or from circulatory collapse, with similar numbers in the two groups. Per protocol analysis did not substantially change results.
“The current findings support the results from the randomized Coronary Angiography after Cardiac Arrest (COACT) trial, which showed no significant differences in clinical outcome among patients with OHCA between immediate and delayed coronary angiography at 90 days and at 1 year,” Desch and colleagues wrote.
“The results of the TOMAHAWK trial very much reinforce the results of COACT,” noted Jorrit Lemkes, MD, of Amsterdam University Medical Center, who led the COACT study but was not involved with TOMAHAWK, in an email to BreakingMED.
“New in TOMAHAWK is that the study looked at patients with all types of arrest rhythms, while COACT only investigated patients with a shockable rhythm. In the TOMAHAWK trial, almost half of patients had a non-shockable rhythm at the time of arrest,” Lemkes wrote.
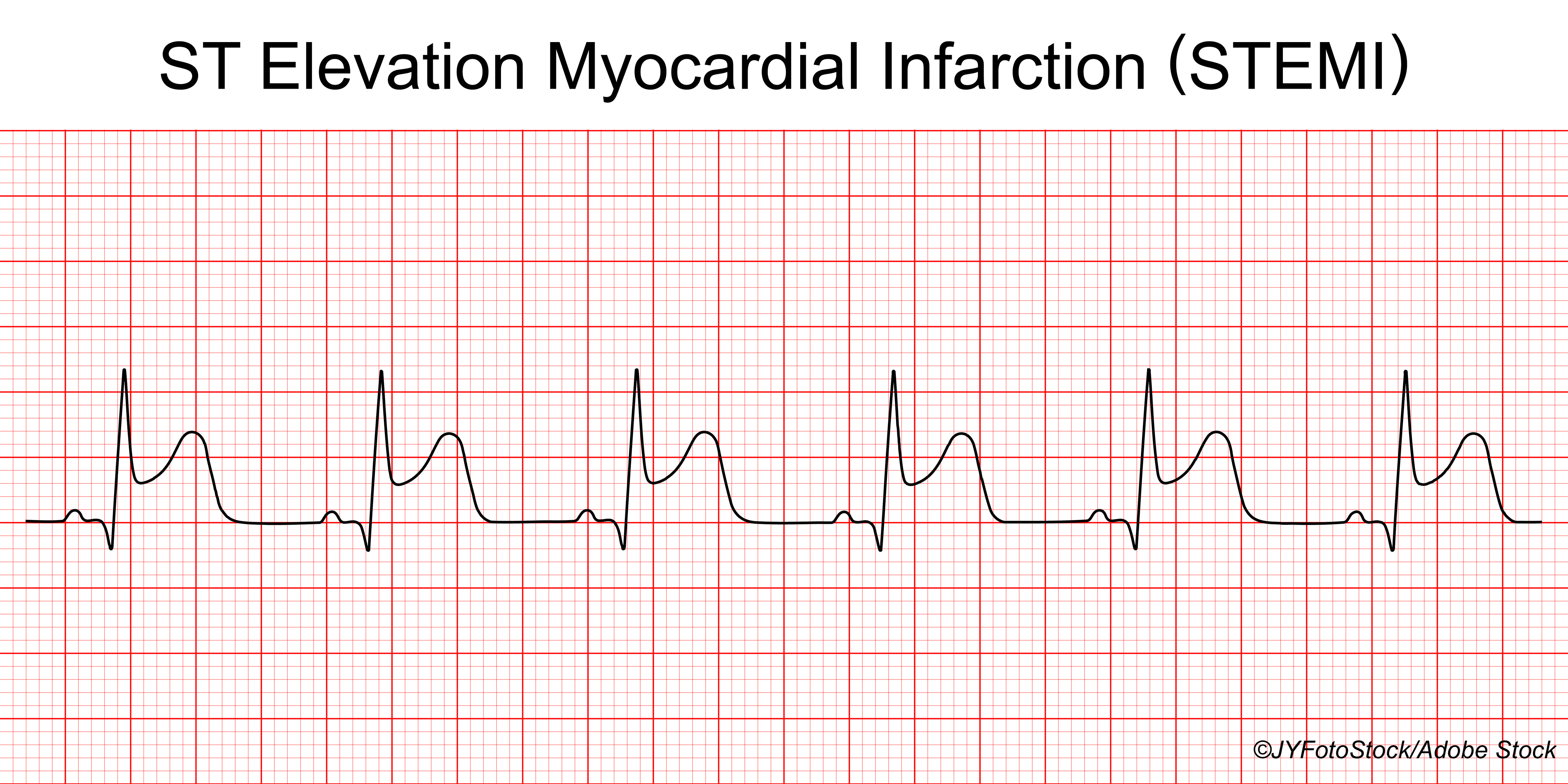
“This might also explain the lower overall survival in TOMAHAWK compared to COACT,” he added. “The TOMAHAWK study supports a wait-and-see approach with respect to coronary angiography in patients after cardiac arrest without ST segment elevation on the ECG and adds force to recent changes in guidelines addressing the treatment of patients who suffered from out-of-hospital cardiac arrest.”
American College of Cardiology Vice-President-elect B. Hadley Wilson, MD, said the TOMAHAWK findings are important because in “the majority of patients that present to emergency departments following out-of-hospital resuscitation—I want to say maybe 60% of cases—the cause of the arrest is not acute MI” thus there is no “need for speed” in getting them to the cath lab.
“What is really interesting about this study is that in the U.S. we are seeing treatment all over the map,” Wilson, who is Executive vice-chair at the Sanger Heart & Vascular Institute/Atrium Health in Charlotte, North Caroline, said in a phone interview. “A large contingent of these patients are taken directly to the cath lab, but these findings show that we can pause, which is potentially safer, before deciding whether or not angiography is needed.”
Another consideration is resource use, Wilson, who was not involved in the trial, explained. “We won’t need to tax our resources, which is especially important in this pandemic era. It reduces the need for 24/7 coverage of the cath lab.”
TOMAHAWK investigators studied 554 patients (mean age 70, 30% women) randomized from November 2016 through September 2019 to either the immediate group (n=281; transferred to the angiography suite as soon as possible after admission) or the delayed group (n=273; transferred to the ICU for further evaluation and treatment at the treating physician’s discretion). A total of 530 patients were included in the primary analysis.
All patients were resuscitated from arrest to an initial ECG rhythm, which was classified as shockable or non-shockable; 55.5% had a shockable arrest rhythm. Overall, the median time from arrest to return of circulation on resuscitation was 15 minutes and the median Glasgow Coma Scale score on admission was 3, indicating the patient was unresponsive.
For the immediate and delayed groups, respectively: angiography was done in 95.5% and 62.2%, median time from arrest to angiography was 2.9 hours and 46.9 hours, and coronary artery disease prevalence in those who underwent angiography was about 61% and 72%. One or more causative lesions were found in 38% and 43%, respectively, and revascularization was done in about 37% and 43%.
Peak troponin and creatinine levels and ICU stay length were similar in the two groups, and no significant group difference was seen in subgroup analysis by age, targeted temperature management, time from arrest to return of spontaneous circulation, or presence of myocardial infarction as arrest trigger. Secondary safety endpoints (moderate or severe bleeding, stroke, need for renal replacement therapy) were also similar between groups.
A composite secondary endpoint, death from any cause or severe neurologic deficit, occurred more frequently in the immediate group (RR 1.16; 95% CI 1.00-1.34), though the rate of severe neurologic deficit alone was not significantly different (18.8% versus 12.7%; RR 1.48, 95% CI 0.82-2.67).
“A possible cause would be that immediate coronary catheterization could lead to delays in diagnosing other triggers of out-of-hospital cardiac arrest,” Desch and co-authors suggested.
ST elevation on post-resuscitation ECG suggests an acute causative lesion for arrest that angiography can localize and address. Non-ST elevation events may be due to other treatable causes. For example, a 2020 study found an increase in OHCA with exposure to California wildfires between 2015 and 2017.
In people OHCA but no ST elevation, immediate angiography may therefore delay diagnosis and treatment of a non-acute coronary syndrome etiology while conferring no possible benefit. How to determine which non-ST elevation patients can benefit from angiography and intervention remains an area of active research. In addition to COACT, a 2018 observational study of OHCA of presumed cardiac cause found that use of early angiography varied by a prognosis risk score, with rates of 86%, 66%, and 47% in low, medium, and high risk patients, respectively. Only the low-risk group had survival benefit.
The lack of benefit seen for immediate angiography might be due in part to an etiologically diverse non-ST elevation OHCA cohort likely to contain patients with arrest triggers other than those addressed by angiography and revascularization, Desch and colleagues suggested. It may also be due in part to the neurologic injury commonly seen with the hypoperfusion accompanying arrest.
“Neurologic rather than cardiac injury may have the most substantial effect on overall prognosis in many patients with cardiac arrest, thereby attenuating a possible beneficial effect of coronary revascularization,” they noted. “Brain injury was by far the most frequent cause of death among the patients in our trial.”
Both considerations, along with only modest sensitivity and specificity for many proposed markers of a treatable culprit lesion in OHCA without ST elevation point to “the necessity of further refinements in selecting the appropriate patients for cardiac catheterization,” Desch and co-authors wrote.
Limitations of the trial included non-blinded treatment assignments, which may have affected treatment decisions.
-
Immediate coronary angiography after successful resuscitation for out-of-hospital cardiac arrest without ST elevation showed no all-cause 30 day mortality benefit versus delayed angiography in the open-label TOMAHAWK trial.
-
A composite secondary endpoint, death from any cause or severe neurologic deficit, occurred more frequently in the immediate angiography group.
Paul Smyth, MD, Contributing Writer, BreakingMED™
The study was supported by the German Center for Cardiovascular Research.
Desch had no disclosures.
Cat ID: 358
Topic ID: 74,358,730,358,192,925



Create Post
Twitter/X Preview
Logout