In subsequent screenings, and when stratified according to breast density, women in both nondense and dense breast tissue categories continued to benefit from improved recall and cancer detection rates with DBT. However, researchers found that there was no such benefit shown for women with extremely dense breast tissue.
The study, led by Kathryn P. Lowry, MD, Department of Radiology, University of Washington, Seattle Cancer Care Alliance, Seattle, was published in JAMA Network Open.
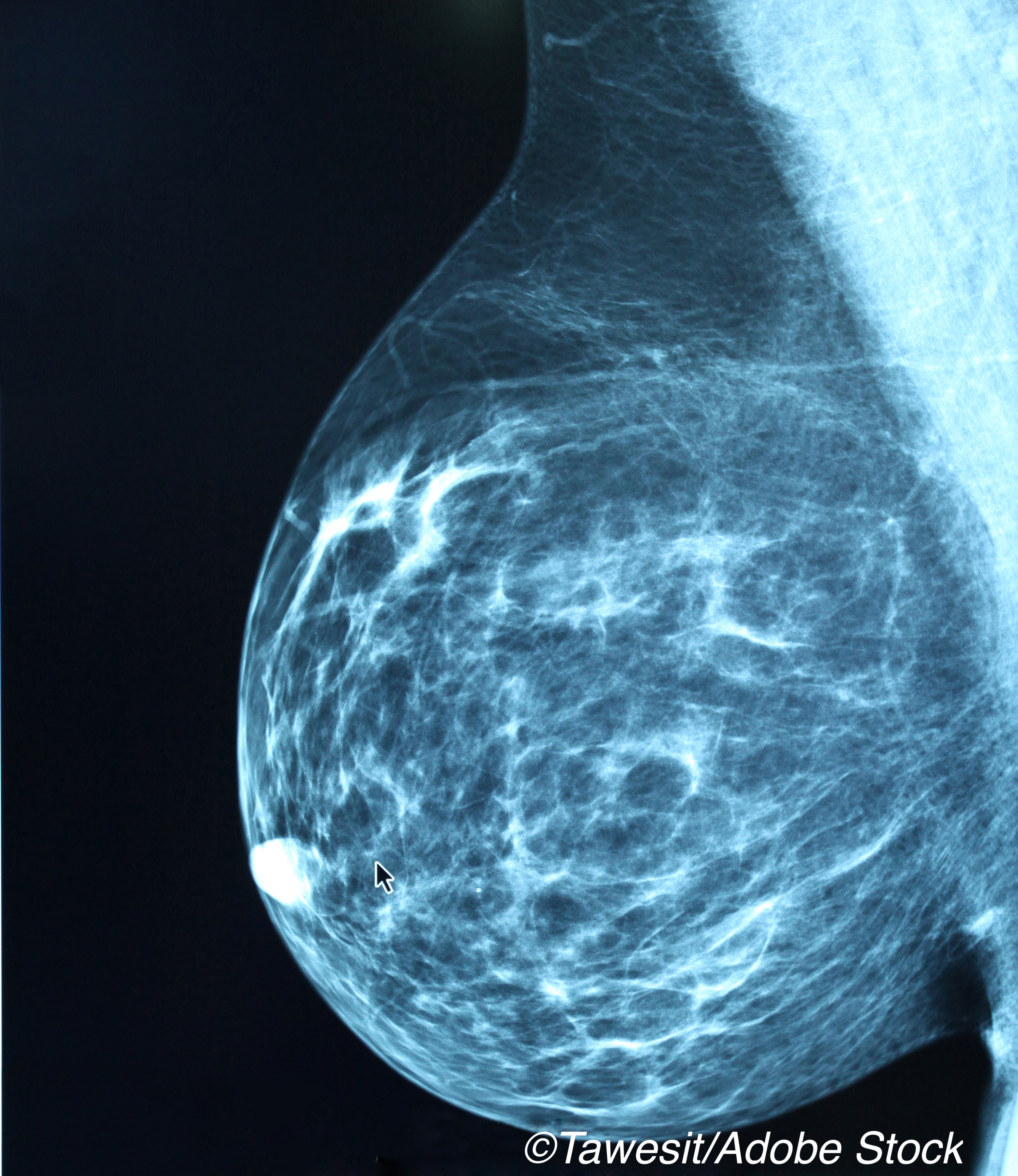
DBT has rapidly become part of routine cancer screening and has been shown to improve performance compared to digital mammography. However, according to Lowry and colleagues, some questions remain about its effectiveness, such as how outcomes vary by breast density or age or vary on baseline versus subsequent screening.
“These questions are important to address during this period of transition to DBT while many centers are currently unable to offer DBT to all women undergoing screening,” wrote Lowry and colleagues.
In addition, the authors noted that physician surveys suggest that many of them perform DBT on women with dense breasts and other breast cancer risk factors even though the data is insufficient to support these practices. In this study, the objective was to compare the performance of digital mammography (DM) to DBT according to age, breast density, and baseline versus subsequent screenings.
This comparative effectiveness study assessed 1,584,079 screening examinations across 46 US facilities (1,273,492 DM and 310,587 DBT).
Lowry and colleagues found that the largest adjusted differences in performance between DM and DBT were seen on baseline examinations. Specifically, they determined that per 1,000 baseline examinations:
- Screening recalls decreased from 240 for DM to 215 for DBT in women aged 40 to 49 years (RR, 0.90; 95% CI, 0.80-1.01).
- Screening recalls decreased from 241 for DM to 204 for DBT in women aged 50 to 59 years (RR, 0.84; 95% CI, 0.73-0.98).
- Screening recalls decreased from 219 for DM to 178 for DBT in women aged 60 to 79 years (RR, 0.80; 95% CI, 0.69-0.95).
In addition cancer detection rates per 1000 examinations increased from 3.2 for DM to 4.4 for DBT in women aged 40 to 49 years (RR, 1.41; 95% CI, 1.11-1.80), from 5.9 for DM to 8.8 for DBT in women aged 50 to 59 years (RR, 1.50; 95% CI, 1.10-2.08), and from 10.8 for DM to 15.1 for DBT in women aged 60 to 79 years (RR, 1.42; 95% CI, 1.09-1.86). Higher invasive cancer detection was also achieved with DBT across all age groups.
According to Lowry and colleagues, these large absolute improvements with DBT indicate the importance of prioritizing DBT screening for women undergoing breast cancer screening for the first time.
Those differences between DM and DBT varied by age and density subgroups when it came to subsequent examinations.
The recall rate was lower with DBT for women with scattered fibroglandular density and heterogeneously dense breasts in all age groups. For example, in women aged 50 to 59 years with scattered fibroglandular density, the number of recall examinations decreased from 102 with DM to 93 with DBT (RR, 0.91; 95% CI, 0.84-0.98).
Cancer detection rates were also higher for subsequent DBT examinations compared with DM in women with heterogeneously dense breasts, with gains increasing by age — 2.5 to 3.1 in women age 40 to 49 years (RR, 1.28; 95% CI, 1.02-1.61), from 3.7 to 5.3 in women age 50 to 59 (RR, 1.42; 95% CI, 1.23-1.64), and from 6.1 to 8.5 in women age 60 to 79 years (RR, 1.39; 95% CI, 1.25-1.54). Total cancer detection rates were also higher for DBT than for DM in women with scattered fibroglandular density at 50 to 79 years of age.
However, Lowry and colleagues observed no improvements in recall or cancer detection rates in women with extremely dense breasts on subsequent examinations for any age group.
In a commentary accompanying the study, Catherine M. Tuite, MD, Fox Chase Cancer Center, Philadelphia, and colleagues, wrote that its results suggest that women with extremely dense breast tissue may benefit more from supplemental screening than women with heterogeneously dense breast tissue.
“Research to determine density and risk-specific outcomes for supplemental screening methods, such as magnetic resonance imaging (including abbreviated protocols), molecular breast imaging, or ultrasonography is necessary to understand which screening method beyond DBT is best for average-risk women with heterogeneous or extremely dense breasts,” they wrote.
And, noting that DBT is more expensive that digital mammography, Tuite and colleagues suggested that the results of this study “may help inform discussions between women and their physicians about how best to use limited health care resources.”
-
Digital breast tomosynthesis results in fewer recalls and higher breast cancer detection rates than digital mammography at baseline screening.
-
These benefits may vary by age and breast density category with subsequent screenings, with no apparent benefit seen for women with extremely dense breast tissue.
Michael Bassett, Contributing Writer, BreakingMED™
Lowry reported receiving grants from GE Healthcare outside the submitted work.
Cat ID: 481
Topic ID: 95,481,730,22,691,192,925,481

