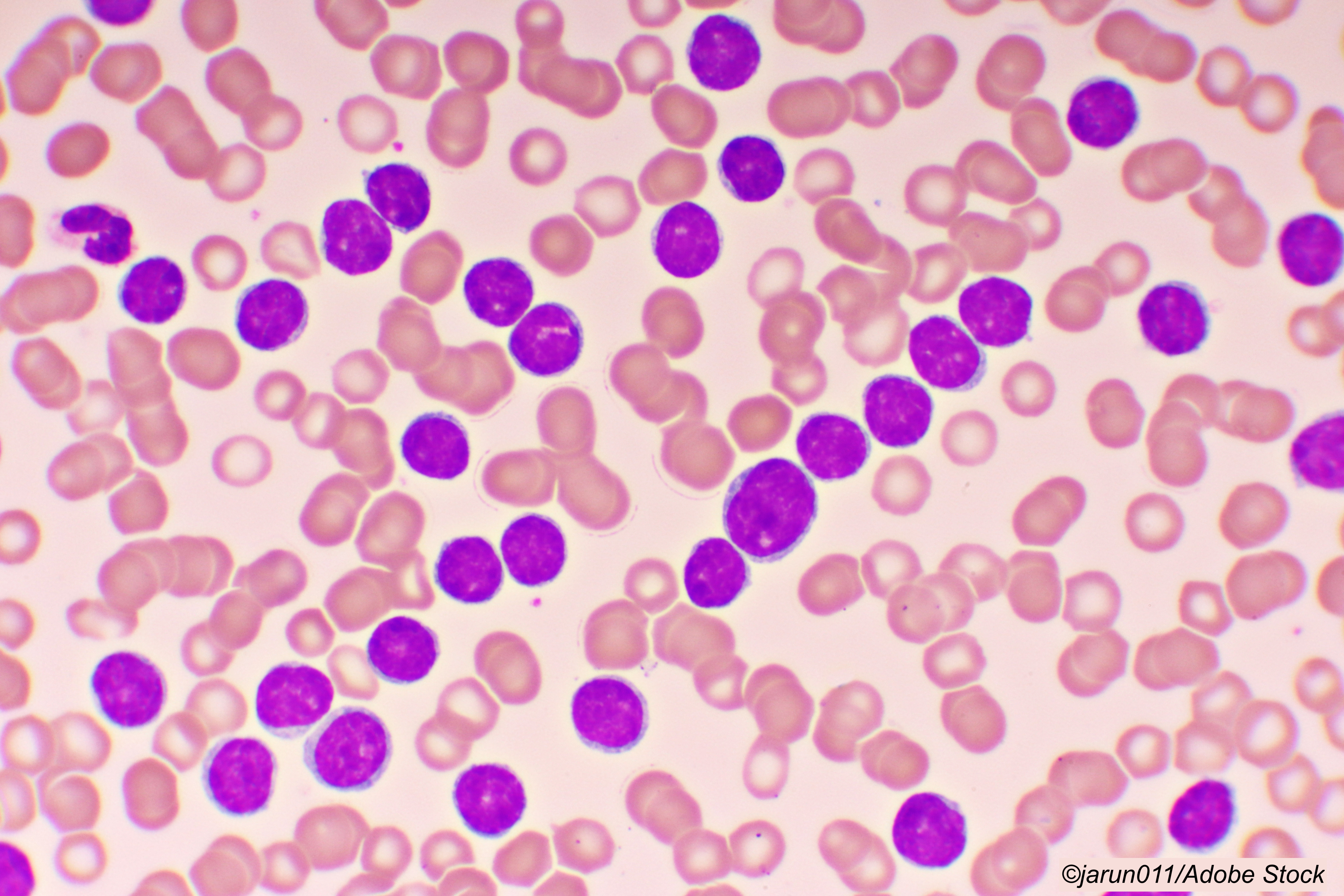
ATLANTA—After two years of follow-up, patients diagnosed with chronic lymphocytic leukemia (CLL) who achieved undetectable minimal residual disease with the combination of ibrutinib and venetoclax appeared to maintain remission, even after discontinuing maintenance treatment with ibrutinib, researchers reported here.
In the updated results of the phase II CAPTIVATE study, Paolo Ghia, MD, PhD, Università Vita-Salute San Raffaele and IRCCS Ospedale San Raffaele, Milano, Italy, reported no new minimal residual disease relapses, no progressive disease, and no death among patients with confirmed undetected residual disease who were then treated with placebo or ibrutinib.
The two-year disease-free survival rates post-randomization remained unchanged at 95% among the patients who were switched to placebo compared with 100% of the patients assigned to ibrutinib maintenance, for a 4.7% difference (P=0.1573), Ghia said in his oral virtual presentation at the American Society of Hematology 2021 meeting.
“The results in patients with confirmed undetectable minimal residual disease support the potential for treatment-free remission with fixed-duration treatment, including in patients with high-risk features,” Ghia said.
Moreover, the three-year progression free survival from the start of the study treatment was at least 95% in all the minimal residual disease-directed, randomized treatment arms, he said. “Early data suggest that patients who progress after fixed duration treatment with ibrutinib plus venetoclax can be successfully retreated with single-agent ibrutinib,” Ghia said.
In addition to maintaining remission, he also noted that there didn’t seem to be a cost in adverse events. “With median study follow-up of 38 months, adverse events remained consistent with known profiles for single agent ibrutinib and venetoclax,” he said. “No new safety issues emerged.” He reported that after 48 months of treatment, 13% of patients discontinued due to adverse events.
In commenting on the study, Shuo Ma, MD, PhD, of Northwestern University School of Medicine, Chicago, told BreakingMED that “The study shows that both the patients who remained on treatment and those who were on placebo did very well. That seemed to be the outcome across all the arms in this study.
“It does offer hope that when these patients reach an undetectable minimal residual disease we may be able to offer them a durable drug holiday, and then if disease is detected we can still re-treat them,” Ma added.
Ghia noted that the two agents—a Bruton tyrosine kinase inhibitor (ibrutinib) and an oral BCL-2 inhibitor (ventoclax)—have previously demonstrated efficacy as a single-agent first-line treatment (ibrutinib) or as either monotherapy or in combination with rituximab or obinutuzumab, in the case of ventoclax.
The fact that the agents have distinct and complementary mechanisms of action means they work synergistically to mobilize chronic lymphocytic leukemia cells from lymph nodes and lymphoid niches, enhance cell killing, and eliminate distinct chronic lymphocytic leukemia cell populations, Ghia explained.
The researchers designed CAPTIVATE, an international, multicenter, phase II study, to evaluate if patients who achieved undetectable minimal residual disease could stop taking the ibrutinib-based therapy after a fixed duration of therapy. At one year, 100% of the patients who remained on the treatment regimen achieved confirmed undetectable minimal residual disease, as did 95% of the patients who were switched to placebo—essentially on a drug holiday.
Ghia and colleagues enrolled 164 patients, median age 58, with previously untreated chronic lymphocytic leukemia. Many of the patients were at high risk for progressive disease including unmutated IGHV; 17p deletion/TP53 mutation; complex karyotype; and del(11q) without del(17p).
The patients were administered three cycles of ibrutinib as a lead-in, which was followed by 12 cycles of combined oral ibrutinib at a dose of 420 mg/day, plus oral venetoclax at 400 mg/day, for a total of 15 cycles. During cycle 16, there were 86 patients with confirmed minimal residual disease in both peripheral blood and bone marrow who were randomized 1:1 to receive double-blind treatment with placebo or single-agent ibrutinib maintenance therapy. Median overall follow-up was 38.2 months. Median post-randomization follow-up was 24 months.
-
In a randomized phase II trial, chronic lymphocytic leukemia (CLL) patients who achieved undetectable minimal residual disease after treatment with ibrutinib and venetoclax maintained remission on placebo.
-
These results were reported at a medical meeting, and the findings should be taken with caution until they are published in a peer reviewed journal.
Edward Susman, Contributing Writer, BreakingMED™
Ghia disclosed consultant fees, honoria, and/or grant support from Janssen, Gilead, Celgene/Juno/BMS, BeiGene, Roche, AbbVie, Acerta/AstraZeneca, ArQule/MSD, and Sunesis.
Ma disclosed research funding, honoraria, or speaker’s bureau fees from Loxo, AstraZeneca, Juno, Beigene, Janssen, TG Therapeutics, and Pharmacyclics.
Cat ID: 118
Topic ID: 78,118,730,118,119,332,466,935,192,925,331