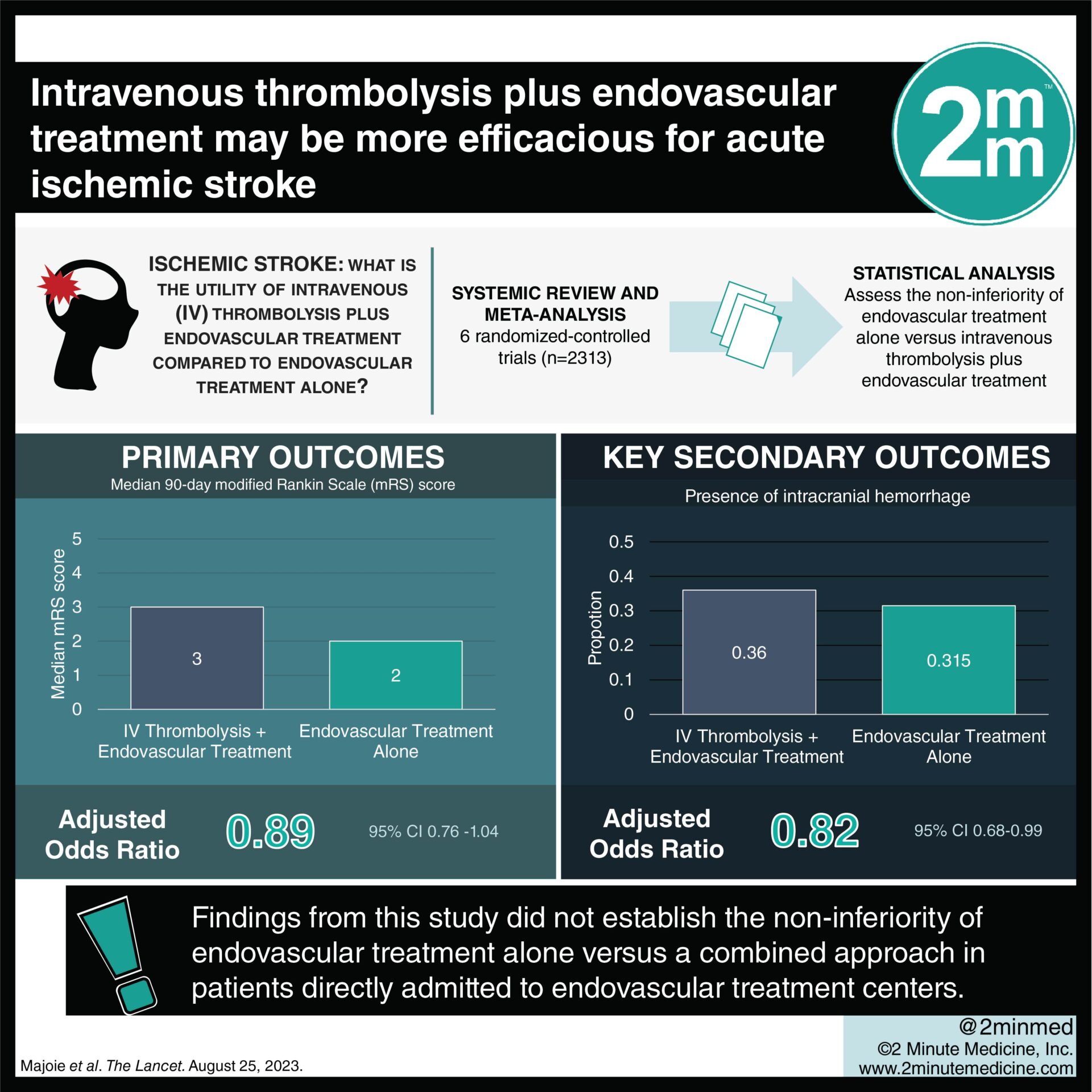
1. The 90-day modified Ranking Scale score was comparable for patients in intravenous thrombolysis plus endovascular treatment versus endovascular treatment alone.
2. Intracranial hemorrhage was less frequent in the endovascular treatment alone group.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Intravenous thrombolysis before endovascular treatment is the preferred therapy among patients with acute ischemic stroke; however, its utility among patients directly admitted to endovascular treatment centers remains unknown. This systematic review and meta-analysis aimed to assess the non-inferiority of endovascular treatment alone versus intravenous thrombolysis plus endovascular treatment. The primary outcome was a 90-day modified Rankin Scale (mRS) score, while the key secondary outcome was the presence of intracranial hemorrhage. According to study results, non-inferiority could not be established between endovascular treatment alone and intravenous thrombolysis plus endovascular treatment. Any-grade intracranial hemorrhage was less common with the endovascular treatment alone group, but symptomatic intracranial hemorrhage did not differ between groups. Thus, although this study was well done, it was limited by the absence of a definitive conclusion about the efficacy of both treatments among patients admitted directly to endovascular treatment centers.
Click to read the study in The Lancet
Relevant Reading: Thrombolysis Guided by Perfusion Imaging up to 9 Hours after Onset of Stroke
In-depth [systematic review and meta-analysis]: A total of 6 randomized-controlled trials (n=2313, 1153 in endovascular treatment alone and 1160 in intravenous thrombolysis and endovascular treatment) were included from database inception to Mar 9, 2023. The primary outcome of median 90-day mRS score was comparable for endovascular treatment and intravenous thrombolysis plus endovascular treatment (3 vs. 2, adjusted odds ratio [aOR] 0.89, 95% confidence interval [CI] 0.76-1.04). Intracranial hemorrhage was less frequent in the endovascular treatment alone group (aOR 0.82, 95% CI 0.68-0.99). However, there were no significant differences in symptomatic intracranial hemorrhage and mortality rates. Findings from this study suggest that the non-inferiority of endovascular treatment alone versus a combined approach in patients directly admitted to endovascular treatment centers was not established.
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.