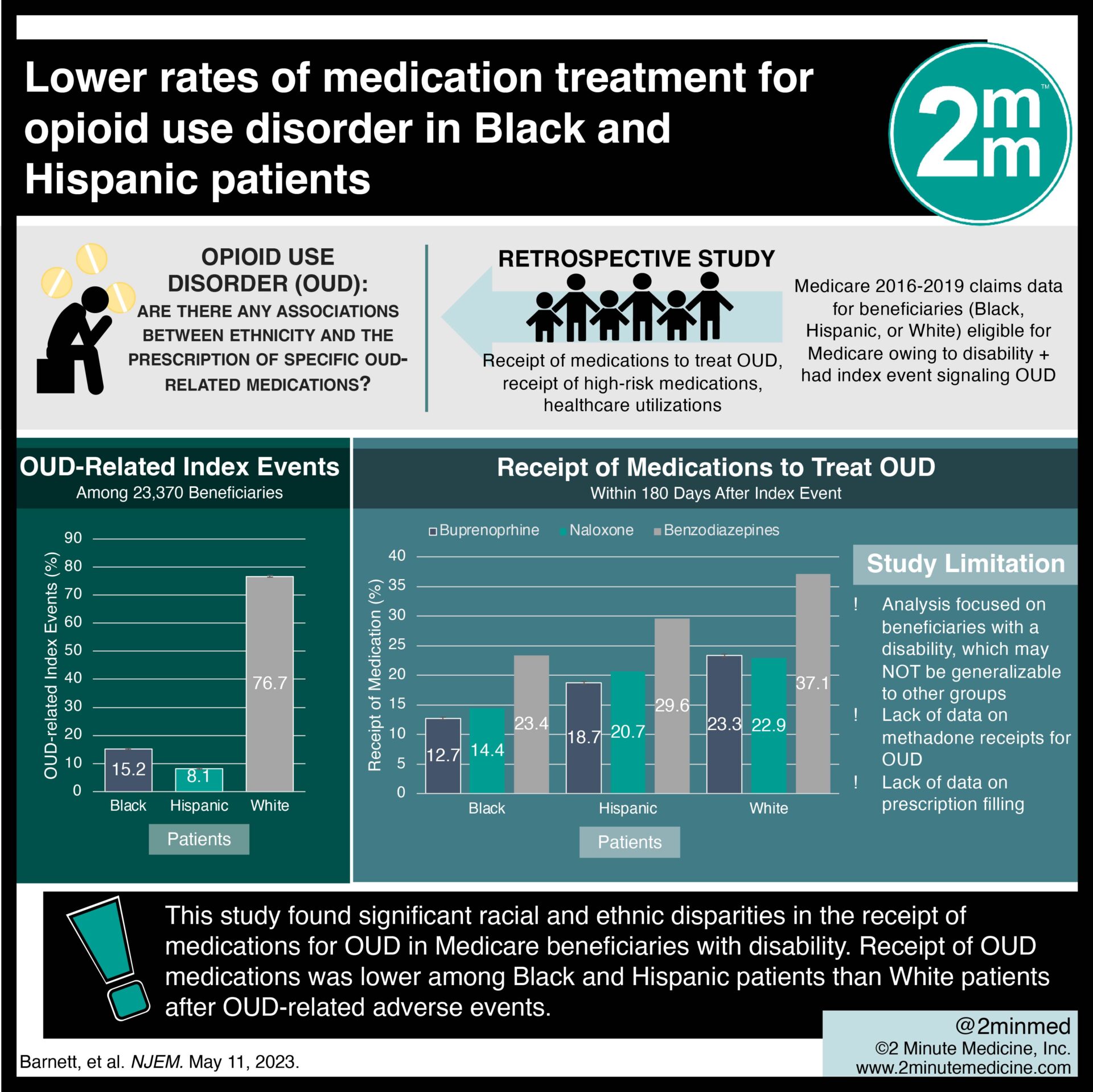
 1. In this retrospective study of Medicare claims data from 2016 to 2019, receipt of opioid use disorder (OUD) medications (buprenorphine and naloxone) was lower among Black and Hispanic patients than White patients after OUD-related adverse events.
1. In this retrospective study of Medicare claims data from 2016 to 2019, receipt of opioid use disorder (OUD) medications (buprenorphine and naloxone) was lower among Black and Hispanic patients than White patients after OUD-related adverse events.
2. Analysis of available methadone receipt data from 2020 to 2021 showed that Black patients received either buprenorphine or methadone at a lower rate than Hispanic or White patients after OUD-related adverse events.
Evidence Rating Level: 2 (Good)
Study Rundown: Rates of opioid overdose are rising for Black and Hispanic populations in the United States. These marginalized populations are less likely than White individuals to receive medications for OUD, access appropriate healthcare, and continue OUD treatment. There is a paucity of evidence on the associations between ethnicity and the prescription of specific OUD-related medications or drugs associated with higher overdose risks. In this retrospective study, Medicare claims data were collected from 2016 to 2019 of adults eligible for Medicare owing to disability with an index event signaling active OUD symptoms. Patients were followed for 180 days after the index event. For the primary outcome, significantly lower percentages of index events among Black and Hispanic patients than among White patients were followed by receipt of buprenorphine, naloxone, or benzodiazepine. Methadone data could not be included in the overall analysis, as it was only included in the Medicare coverage expansion in 2020. However, Black patients did receive either buprenorphine or methadone less frequently after the index event than White patients in the 2020 to 2021 analysis. For limitations, the analysis focused on beneficiaries with a disability, which may not be generalizable to other groups. Other limitations include the lack of data on methadone receipts for OUD and the lack of data on prescription filling.
Click here to read the study in NEJM
In-Depth [retrospective cohort]: In this retrospective cohort study, Medicare claims data were collected from 2016 to 2019 for adults eligible for Medicare owing to disability with an index event signaling active OUD symptoms. Patients were followed for 180 days after the index event. In total, the study included 23,370 beneficiaries, classified as Black (n=3,524), Hispanic (n=1,858), and White (n=17,988), respectively. There were 25,904 OUD-related index events (15.2%, 8.1%, and 76.7% were Black, Hispanic, and White patients, respectively). Black (-8.7 percentage points; 95% Confidence Interval [CI], -11.3 to -6.0) and Hispanic patients (-4.2 percentage points; 95% CI, -6.7 to -1.8) were less likely to receive any buprenorphine than White patients. In addition, Black patients received lower days’ supply and had poorer treatment retention than White patients. This race effect on medication receipts was mediated by past OUD medication fills. No difference was found for naloxone receipts. Black patients received fewer buprenorphine or methadone medication receipts compared to White patients. For high-risk medications, no difference in opioid analgesic receipts was found between groups. For benzodiazepines, the incidence of receipt was lowest among Black patients and highest among White patients. For health care utilizations, Black and Hispanic patients index events were followed by fewer ambulatory visits. Black patients had more emergency department visits and hospitalizations compared to White patients. This study found significant racial and ethnic disparities in the receipt of medications for OUD in Medicare beneficiaries with disability.
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.








