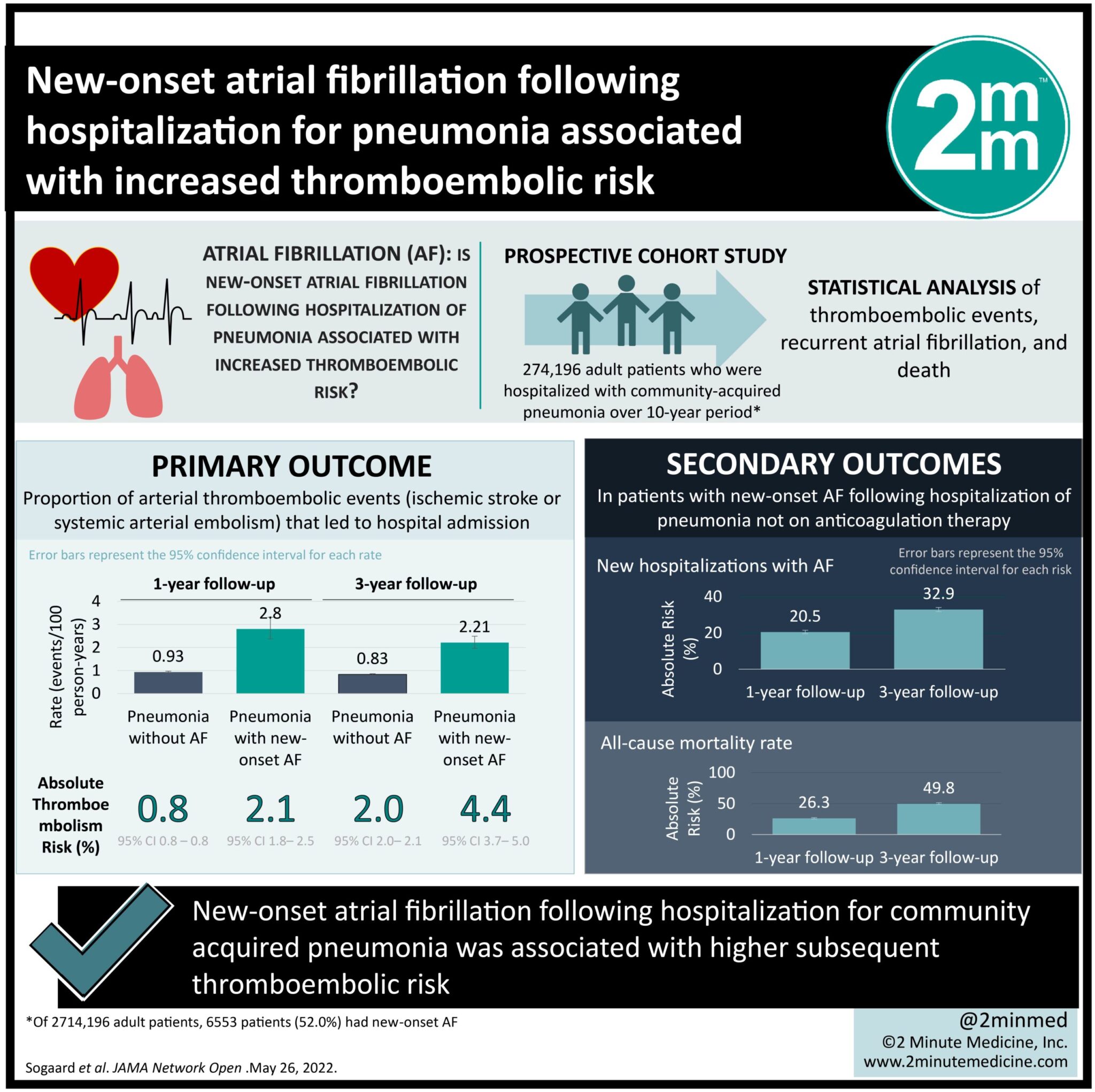
1. New-onset atrial fibrillation following hospitalization for community acquired pneumonia was associated with higher subsequent thromboembolic risk.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Atrial fibrillation (AF) is a known complication in 4-10% of patients with pneumonia. Stroke risk may exceed that of the general population with AF, but clear guidelines are lacking for anticoagulant treatment decisions in these patients. A Danish population cohort study aimed to examine the thromboembolic risk in patients with new-onset AF following infection with pneumonia. The study included 274 196 adult patients who were hospitalized with community-acquired pneumonia, with enrolment over a 10-year period. Within this group, 6553 patients (52.0%) had new-onset AF. In patients not receiving anticoagulation, the 1-year thromboembolism risk was 2.1% in patients with AF compared to 1.8% in those without AF (95% CI, 1.8%-2.5%). At three years, the all-cause mortality rate was 49.8% in patients with pneumonia and new-onset AF (95% CI, 48.6%-51.1%) compared to 25.7% (95% CI, 25.6%-25.9%) in patients with pneumonia without AF. These findings suggest that AF and thromboembolic risk following acute infection may not be a transient phenomenon and further risk-benefit analysis of therapeutic anticoagulation may be warranted.
Click here to read the story in JAMA
Relevant Reading: New-onset atrial fibrillation among patients with infection in the emergency department: A multicenter cohort study of 1-year stroke risk
In-Depth [Prospective cohort study]: The source population was drawn from 3 Danish linked registries. Patients with prior diagnoses of AF and treatment with anticoagulation within 180 days were excluded, as were patients who initiated treatment or died during the landmark period of 30 days. Follow-up continued from a 30-day landmark period to a maximum of 3 years. Primary outcomes included proportions of arterial thromboembolic events that led to hospital admission (either stroke or systemic arterial embolism). Secondary outcomes were recurrent hospital or outpatient clinic contacts with AF, oral anticoagulant therapy initiation and all-cause mortality at 1 and 3 years of follow-up. Each patient’s stroke risk was determined using the CHA2DS2-VASc score. It was found that most patients with new-onset AF had an intermediate or high CHA2DS2-VASc score (94%). Furthermore, stroke risks in patients with intermediate or high risk were 1.4% (95% CI, 1.0%-2.0%) and 2.8% (95% CI, 2.3%-3.4%), respectively. At three years, 32.9% of patients had AF at new hospitalizations (95% CI, 31.8%-34.1%) and 14.0% had begun anticoagulation therapy (95% CI, 13.2%-14.9%). Stroke risk at three-year follow up was 3.5% (95% CI, 2.8%-4.3%) in patients with intermediate risk, and 5.3% (95% CI, 4.4%-6.5%) in those with high stroke risk, respectively.
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.