Evidence Rating Level: 1 (Excellent)
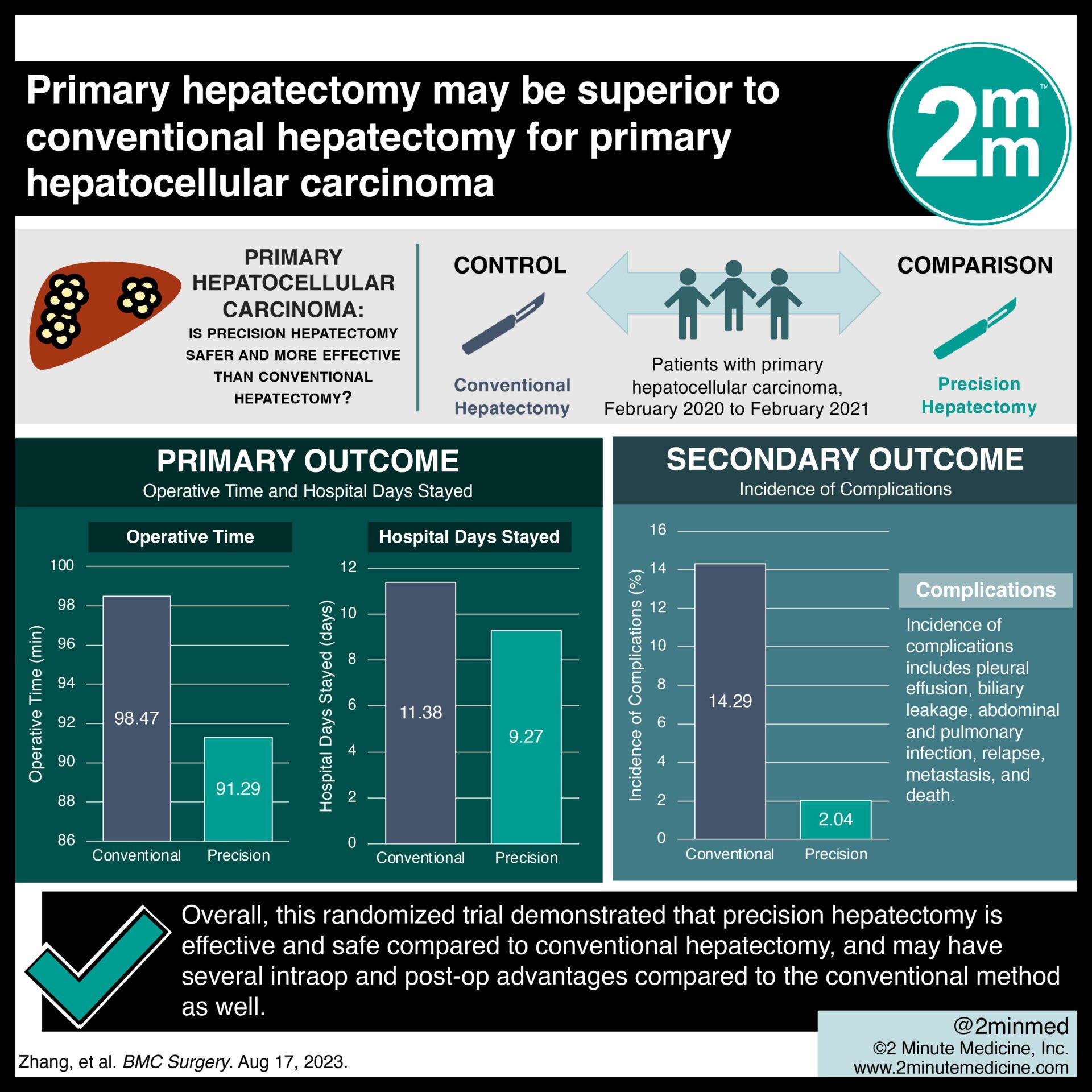
For patients with primary liver cancer, precision hepatectomy is a novel surgical approach that aims to decrease invasiveness and improve hepatic protection: This is done by creating a virtual 3D reconstruction of an individual patient’s liver to guide the surgical plan. This current randomized controlled trial compared the outcomes of patients undergoing conventional versus precision hepatectomy for primary hepatocellular carcinoma. This was a single-centre trial based in China, with 49 patients in the conventional hepatectomy (control) group and 49 in the precision hepatectomy (study) group. In the study group, CT scans were used to virtually reconstruct each patients’ livers, and various surgical options were analyzed using these reconstructions, to inform the surgical plan prior to surgery. The outcomes measured included operation time, complications, liver and immune function 1 week post-op, and recurrence or metastasis, with follow-up done up to 3 years after surgery. The results showed that in the study group compared to the control, there was significantly less operation time (91.29 vs 98.47 min), less intraoperative bleeding (220.71 vs 248.91 mL), less anal venting time (72.19 vs 81.23 h), and fewer hospital days stayed (9.27 vs 11.38; all p < 0.001). There were significantly higher levels of CD4+, CD3+, and CD4+/CD8+ in the study compared to control 1-week post-op (p < 0.001). In the study group, there were also higher levels of ALT (32.81 vs 26.98), AST (41.38 vs 43.98), total bilirubin (17.47 vs 14.39), and albumin (55.39 vs 46.19) 1-week post-op. As well, there was a lower incidence of complications in the study versus control group (2.04% vs 14.29%, p = 0.027). Lastly, there was a significantly lower incidence of relapse (2.04% vs 14.29%, p = 0.027) and death (2.04% vs 14.29%, p = 0.027) in the study compared to control group, with no difference in metastasis (2.04% vs 8.16%, p = 0.168). Overall, this randomized trial demonstrated that precision hepatectomy is effective and safe compared to conventional hepatectomy, and may have several intraop and post-op advantages compared to the conventional method as well.
Click to read the study in BMC Surgery
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.















