1. Patients receiving secukinumab every 2-weeks showed superior clinical response rates compared to those receiving placebo.
2. Secukinumab was well-tolerated, and the most common adverse effect was a headache.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Hidradenitis suppurativa is an inflammatory dermatological condition that leads to abscesses and scarring of the skin. Current treatment typically includes topical medication and surgical intervention. There is only one biologic therapy (adalimumab) approved for the treatment of moderate-to-severe hidradenitis. The SUNSHINE and SUNRISE trials were two identical studies evaluating the use of subcutaneous secukinumab for the treatment of hidradenitis suppurativa. Participants were randomized to receive either placebo, secukinumab every two weeks or secukinumab every four weeks. The placebo-controlled study period was for 16 weeks, followed by a long-term treatment period without a placebo for 52 weeks. In both trials, significantly more patients on secukinumab every 2 weeks had a clinical response compared to placebo, and this benefit was sustained up to 52 weeks. The most common adverse effect in the secukinumab group was headaches and there were no treatment-related deaths. Limitations of this study include a shorter placebo-controlled period. Nevertheless, this study provides evidence for the clinical efficacy of secukinumab every 2 weeks for the treatment of hidradenitis suppurativa.
Click to read the study in The Lancet
Relevant Reading: Efficacy and Safety of Adalimumab in Conjunction With Surgery in Moderate to Severe Hidradenitis Suppurativa
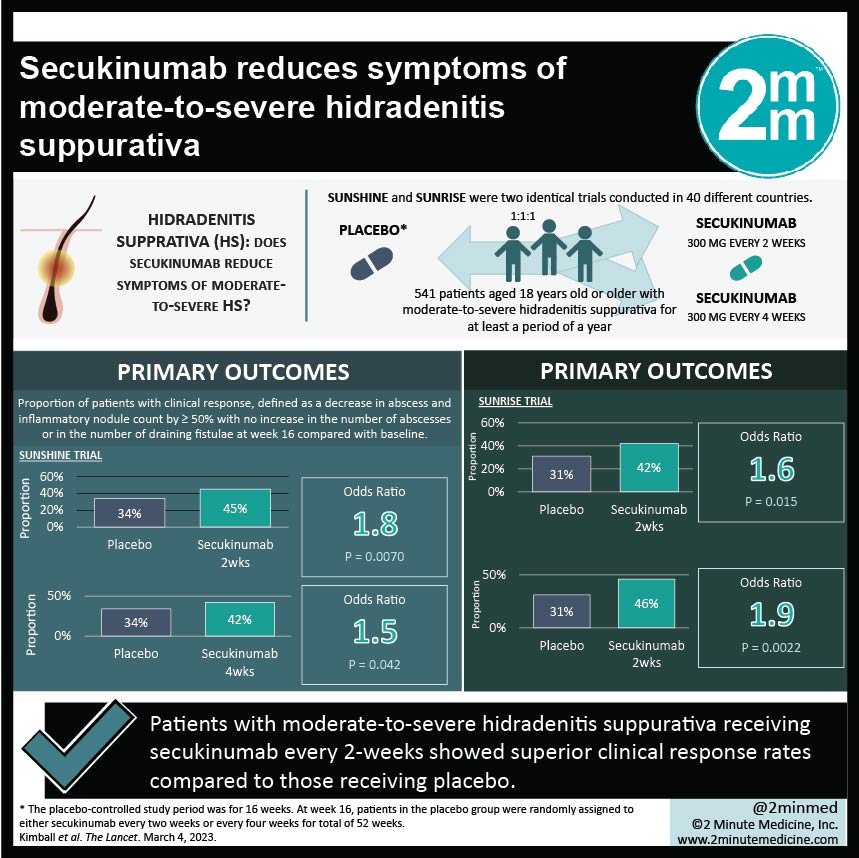
In-Depth [randomized controlled trial]: SUNSHINE and SUNRISE were two identical trials conducted in 40 different countries. Eligible patients were 18 years old or older and had moderate-to-severe hidradenitis suppurativa for at least a period of a year. A total of 541 participants were randomized 1:1:1 to either secukinumab 300 mg every 2 weeks, secukinumab 300 mg every 4 weeks, or to placebo. The study consisted of a placebo-controlled period from week 0 to week 16 (period 1), a long-term treatment period to week 52 (period 2), and a follow-up period to week 60 (period 3). Treatments were given subcutaneously. At week 16, patients in the placebo group were randomly assigned to either secukinumab every two weeks or every four weeks. The primary outcome was the proportion of patients with clinical response, defined as a decrease in abscess and inflammatory nodule count by 50% or more with no increase in the number of abscesses or in the number of draining fistulae at week 16 compared with baseline.
The study contained 304 (56%) women and the mean age of participants was 36.1 years. Significantly more participants in the secukinumab every 2 weeks group had clinical response compared to placebo in both the SUNSHINE (34% in placebo, 45% in secukinumab every 2 weeks, odds ratio 1.8, p=0.0070) and SUNRISE trials (31% in placebo, 42% in secukinumab every 2 weeks, odds ratio 1.6, p=0.015). In the SUNRISE trial, there were significantly more patients with a clinical response on secukinumab every 4 weeks compared to placebo (odds ratio 1.9, p=0.0022); however, there was no significant difference in the SUNSHINE trial. The most common adverse effect in both the SUNSHINE and SUNRISE trial was a headache. There were no study-related deaths.
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.